The Complete Guide To Preventing Mosquito Bites When Travelling (+ Must-Read FAQ)

From rats and cockroaches to fire ants and leeches, most travellers have to deal with annoying pests at some point or another in their journey.
But perhaps no pest is as widespread or as consistently problematic for travellers as the humble mosquito.
The mosquito undoubtedly reigns supreme as the most irritating insect pest that travellers face. So irritating that you’d probably throw a banquet if all the mosquitoes were to one day suddenly vanish off the face of the Earth without a trace.
These flying vampires are hellbent on sucking all the enjoyment out of your otherwise fairy-tale trip; it seems that no matter where you go, they’re there, repeatedly attacking your ankles, feet, legs and other exposed body parts in order to dine on your lifeblood.
The sneaky buggers are also highly adept at avoiding detection, flying in under the radar and then injecting saliva containing enzymes that act as a mild painkiller, so that often you don’t even register the attack until afterwards, when the bite starts to swell up and become itchy.
And that exasperating high-pitched whining sound that mosquitoes make as they hover around your ears while you’re trying to fall asleep in your bed at night? That’s almost as irritating as being made a meal of.
But it’s important to remember that mosquitoes are not merely an irritation or nuisance.
Despite their diminutive size, these airborne pests are anything but innocuous and, in fact, the most fitting word to describe them would perhaps be insidious.
As you probably already know, mosquitoes are vectors for a multitude of dangerous diseases including malaria, dengue, West Nile Virus, Zika virus, chikungunya, yellow fever, filariasis, Japanese encephalitis and many others. Wikipedia has a longer list of them.
These diseases collectively result in approximately 2 million human deaths every year, exacting a significantly higher death toll than that of the second biggest man-killer - other humans - which by comparison only accounts for 475,0000 deaths annually.
In total since the dawn of time, it’s estimated that mosquitoes have taken the lives of some 52 billion people – more lives than have been lost in all the wars of history combined.
Mosquitoes have wiped out entire armies, contributed to the collapse of mighty empires and altered the course of the world’s fate on many occasions.
It’s even believed by some researchers that mosquitoes played a major role in the extinction of the dinosaurs.
Mosquitoes are quite literally the world’s deadliest animal and despite our best efforts at ridding the world of them, we have not yet won the war.
The mosquito's resilience partly stems from its extraordinary ability to genetically mutate and develop resistance against the insecticides we invent to annihilate it.
Unfortunately, there are no reliable vaccines or preventative treatments for the majority of mosquito-borne illnesses, which is why knowing how to keep mosquitoes at bay when you travel is crucial for your health and wellbeing, as well as for your sanity and peace of mind.
In this article we’re going to list and discuss the most effective and proven methods for keeping mosquitoes away and avoiding their bites when you're on the road.
After you’ve read through the solutions, keep reading, as we’ve included a bonus FAQ section in the second part of the article to answer all your most pressing questions about mosquitoes and travel.
The FAQ includes advice on antimalarial medications, mosquito-borne illnesses, vaccinations, treatments for bites and much more!
Table of contents
- How to keep mosquitoes away when travelling
- Practical tips for avoiding mosquito bites
- Products that repel mosquitoes
- Spatial vs topical repellents
- Topical repellents
- Spatial repellents
- How to keep mosquitoes away while at your hotel
- Mosquitoes & travelling FAQ - all your questions answered
- What are mosquitoes?
- How long have mosquitoes been around?
- What is the mosquito life cycle?
- What do mosquitoes feed on?
- When and where are mosquitoes most active?
- How do mosquitoes detect your presence?
- Where do mosquitoes prefer to bite people and why?
- How exactly do mosquitoes bite you?
- How to reduce the itching and swelling caused by mosquito bites?
- Is every traveller equally susceptible to being bitten by mosquitoes?
- What diseases can travellers contract from mosquitoes?
- Are mosquito-borne illnesses vaccine-preventable?
- When should travellers take antimalarials and which drugs are best to take?
- Conclusion
There is a host of strategies that you can employ as a traveller to minimize contact with mosquitoes, hence preserving your sanity and reducing the risk of contracting a mosquito-borne illness.
We’ll cover some easy practical tips, the best products for repelling mosquitoes and lastly we’ll go over how to avoid mosquito bites at your accommodation (where you can’t simply go somewhere else).
#1 - Cover up (with the right clothing) any exposed skin during peak mosquito feeding hours

In tropical and subtropical climes where mosquitoes can be a menace, it’s natural to spend most of your time going around in a t-shirt, shorts and sandals because of the intense heat and humidity.
Such attire makes perfect sense until it’s that time of day when the mosquitoes come out to feed, at which point you suddenly find yourself wide open to attack.
The simple solution is to just cover up the exposed skin on your neck, torso, arms, legs, hands and feet during the hours when mosquitoes come out to feast.
We go into more detail about mosquito feeding hours in the FAQ section below, but basically, most species tend be at their most active at dusk and dawn.
These also conveniently happen to be the coolest hours of the day when you might be feeling a little chilly and thinking about donning a long-sleeved shirt or a pair of long pants anyway.
When covering up to prevent mosquito bites, your clothes should be loose fitting, because mosquitoes can still easily bite through a piece of fabric that’s stretched tight against your skin.
You might want to tuck your shirt into your pants and your pants into your socks too so that you have no chinks in your armour for the mosquitoes to exploit.
Make sure to ditch the sandals too and wear a reasonably thick pair of socks with a pair of shoes instead, as some species of mosquitoes love feet and ankles, and are capable of biting through thin socks.
As regards clothing colour, some sources will claim that bright colours are more attractive to mosquitoes, but the majority say that you should avoid wearing dark colours.
If it is true, it may be because dark clothing absorbs radiates more heat than light clothing, which mosquitoes are sensitive to.
The main thing is that you get into the habit of wearing your mosquito-proof outfit whenever you’re getting up at dawn or heading out in the evenings.
#2 - Avoid entering shaded, sheltered areas

During the hottest hours of the day mosquitoes will retreat to the cover of trees and other shady, sheltered areas where the sun doesn’t penetrate and where the air is relatively still.
They prefer these shaded, windless refuges to avoid death by dehydration in the heat of the sun and also because they are poor pilots in high winds, as anyone that has used an electric fan on high speed to blow them away will attest to.
On hot sunny days in the tropics many travellers will have experienced the sudden barrage of mosquito attacks the moment they stepped out of the harsh sun into the shade of trees in order to cool off.
If you must be near trees, always try to stick to the transition zones or forest edges, where there is more sunlight and the chance that a breeze might be blowing to keep the bugs away.
#3 - Ditch the floral-scented soaps, body washes, deodorants and perfumes

I get it; some travellers don’t want to smell like garbage during their trip. But mosquitoes are attracted to the strong scents of the various personal care products that many travellers apply to their bodies.
Perhaps this is because mosquitoes confuse these fragrances with those of flowers, from which they extract nectar as their primary food source.
In any case, if you want to avoid becoming a magnet for mosquitoes, lay off the smelly stuff and try to use more neutral-smelling products that don’t leave a lingering fragrance on your skin.
#4 - Take regular showers and keep your clothing clean

The logic here is pretty simple; mosquitoes are attracted to compounds in human sweat, so by showering frequently and washing your clothes regularly, you get rid of the lactic acid and other compounds found in human sweat that mosquitoes find appealing.
There will be times during a trip when you just don’t want to cover up your exposed skin, and it's virtually impossible to always avoid entering into mosquito habitats during your daily escapades.
To remain protected at all times, you need to employ some kind of a mosquito repellent - something that actively deters mosquitoes from landing on you or entering your personal space.
Mosquito repellents normally fall into one of two categories – spatial repellents and topical repellents.
Topical repellents are the various creams, balms, lotions and liquid sprays that are applied directly to the skin to discourage mosquitoes and other biting insects from landing on you.
Spatial repellents on the other hand work by creating a protective "cloud" around you that is filled with mosquito-repelling substances like smoke, volatile components of essential oils and pyrethroids. Such compounds are hazardous to mosquitoes and impel them to flee the scene.
Both types of repellents can come in portable forms and can provide protection from bugs no matter where you are, although topical repellents are generally more suitable for when you're out and about, while spatial repellents tend to be better for keeping mosquitoes out of your hotel room.
One of the downsides with topical repellents is that they gradually wear off and have to be re-applied every so often (usually every 6 hours or so). They can also make your skin oily and some products can carry a strong, unpleasant smell.
Spatial repellents can also have some issues, as we shall soon see in more detail. Some types can depend on having electricity, while others can make a room not only hostile to mosquitoes but also to their human occupants.
We'll first look more closely at topical repellents, which are based on one or more of the following active ingredients that have been demonstrated to be effective mosquito deterrents.
#1 - DEET

Chemical formula: C12H17NO
In terms of sheer mosquito-repelling efficacy, it’s pretty hard to beat DEET, which is an acronym for N, N-Diethyl-3-methylbenzamide (also N, N-Diethyl-meta-toluamide), a slightly yellowish, almost colourless liquid that endured as the undisputed champion of mosquito repellents for several decades.
DEET was originally developed for the U.S. army in 1944 by a chemist named Samuel Gertier, who was working with the USDA (United States Department of Agriculture) at the time.
The development of DEET was a reaction to the US army’s harrowing experience of jungle warfare during World War II, following which a need was recognized to better protect soldiers in mosquito-infested jungle environments.
After being initially tested as a pesticide on farms, DEET was adopted by the US military in 1946, but it wasn’t until 1957 that it became available to civilians.
The exact mechanism by which DEET repels mosquitoes is still not clearly understood and has caused much debate among scientists.
The most likely explanation is that DEET confuses the insects by changing the way that their olfactory nerves (located on the mosquito’s antennae) respond to 1-octen-3-ol, an alcohol found in human breath that alerts mosquitoes to our presence.
When DEET disrupts the normal response pattern of these olfactory nerves to 1-octen-3-ol, the mosquito can still smell something, but it isn’t quite sure what, so it leaves us alone.
An important consideration when choosing a DEET-based topical repellent is its concentration, which can range widely from 4% to 100%.
In general, the higher the DEET concentration, the more hours of protection the repellent will provide before its effects wear off, although the concentration has little impact on the repellency strength.
Many experts suggest a concentration of 25-30% DEET as optimal, which should provide around 6 hours of protection in most cases, while formulations with 100% DEET will often claim to provide up to 12 hours of protection.
If you only need 1 or 2 hours of protection, you can use a repellent with a DEET concentration below 10%. Some products also use a "slow-release" formula, which can extend the duration of their effectiveness beyond the usual number of hours.
There have been some health concerns regarding the use of DEET. You definitely don’t want to ingest, directly inhale or get the stuff in your eyes. In rare cases DEET can even cause rashes, irritation and swelling of the skin with regular use.
DEET is not recommended at all for infants that are younger than 2 months old and for infants older than 2 months only the lowest concentrations are safe to use.
DEEt should never be applied to children’s hands as they could accidentally rub the chemical into their eyes or ingest when handling food.
Studies have shown that DEET applied to the skin gets absorbed into the bloodstream, where it gets broken down by the liver and is almost completely eliminated from the body via the urine within 24 hours.
DEET has some other notable drawbacks, such as its ability to dissolve certain plastics, such as those found in sunglasses, the lenses of eyeglasses and watch crystals (the protective transparent covers that protect watch faces). Keep the stuff away from your glasses and watch!
DEET can also damage certain synthetic fabrics such as rayon and spandex, (though it has no effect on cotton, wool or nylon) and it has a distinctive odour that many people can’t stand.
The bottom line is that DEET one of the most effective and popular (some 30% of the U.S population uses it) topical repellents on the market and is used by millions of people every year.
One of the most popular DEET-based repellents on the market is Repel® Insect Repellent Sportsmen Max Formula.
This is a 40% DEET formula in a pump spray bottle that was developed for outdoor enthusiasts and sportspeople who become bug magnets when they start perspiring. The relatively high concentration (40%) of DEET in this formula ensures long-lasting protection from mosquitoes and other bugs.
However, being the potent man-made chemical that it is, DEET doesn’t sit well with everyone. This has led to some people steering clear of DEET-based repellents and opting to use alternatives like the ones we discuss below.
#2 - Picaridin
Chemical formula: C12H23NO3
For over 50 years since it was first developed, DEET enjoyed its reign as the matchless top dog of mosquito repellents.
That was, until a synthetic compound called picaridin was developed by the German pharmaceutical giant Bayer AG in the 1980s. By 1998 it had entered the European and Australian consumer markets by 2005 it had reached the U.S.
Picaridin (also known as icaridin, Bayrepel and KBR 3023) is an odourless, colourless liquid that is based on a natural compound called piperine, which was first isolated in 1819 by Hans Christen Orsted from Piper nigrum, the fruits of which plant become the black and white peppercorns that we use for seasoning our food.
Like DEET, picaridin works as an effective mosquito and general insect repellent, also providing protection against black flies and especially midges (no-see-ums), though DEET is believed to be more effective at deterring ticks.
Unlike DEET, picaridin has no distinctive odour, its preparations don’t leave the skin feeling oily and it won’t dissolve plastics and other synthetic materials.
As with DEET, concentration influences the length of time that picaradin-based repellents will remain effective for. Although concentrations can range from 4% to 100% with DEET, with picaridin they generally range from 7% to 20%.
A low 7% picaridin concentration is roughly equivalent to 10% DEET, while a high 20% provides the same 4-5 hours of mosquito protection as the equivalent concentration of DEET.
As regards health consequences, not a great deal is known about the long-term effects of picaridin as it has only been on the consumer market since 1998.
A small amount of picaridin (less than 6%) is absorbed through the skin when applied and it is broken down and then excreted by the body like DEET after this occurs.
Another consequence of being a relative newcomer to the market is that Picaridin is still only used in a limited number of insect repellent products, although that is slowly changing.
For a Picaridin-based repellent, try Ranger Ready Repellent. This orange-and-bergamot-scented 20% picaridin formulation(orange scented) comes in a small mist spray bottle and can be applied directly to skin, clothing and gear for 8-12 hours of protection against mosquitoes, fleas, midges (no see ums), ticks etc.
#3 - IR3535 (3-[N-butyl-N-acetyl]-aminopropionic acid)
Another potent synthetic bug repellent and one of the big four (DEET, picaridin, IR3535 and oil of lemon eucalyptus), IR3535 or EBAAP was developed in the early 1970’s from a natural amino acid called β-alanine, by the American pharmaceutical giant Merck & Co Inc. Its full chemical name is a mouthful – ethyl butylacetylaminopropionate.
Although it has been marketed in Europe since the mid 70’s, IR3535 was only introduced into the U.S market in 1999, so it’s a latecomer to the new world. It’s commonly used in sunscreens and mosquito repellents, and is currently found in about 150 products worldwide.
Depending on the species of mosquito in question, IR3535 has been shown to be equally or slightly less effective at repelling mosquitoes when compared with DEET and picaridin.
A few studies have shown the chemical to be very effective against ticks. One study found IR3535 to be twice as potent as DEET at repelling nymphal deer ticks (Ixodes scapularis).
The recommended formulation for combatting ticks and mosquitoes is generally 10 to 30 percent IR3535.
As regards safety, IR3535 has a pretty spotless record and European authorities have received few if any complaints about adverse effects caused by the chemical, although it can be irritating to the eyes, and it may also damage or dissolve plastics.
Overall, this is a mosquito repellent to be reckoned with, and will be especially advantageous in situations where dangerous lyme-disease-transmitting ticks are also on the cards.
#4 - Oil of lemon eucalyptus
Crude lemon eucalyptus essential oil is obtained by steam distilling the dried leaves and twigs of Corymbia citriodora, the Australian lemon eucalyptus tree.
Unfortunately this essential oil’s life as a repellent is fleeting (approximately 1 hour) due to the volatile nature of its mosquito-repelling constituents.
However, one component present in the unrefined oil in small quantities is PMD (p-menthane 3,8 diol), which is a very effective and long lasting mosquito repellent.
By increasing the amount of PMD from 1 to 65 percent while also reducing the citronellal content of lemon eucalyptus essential oil, you get a refined product known as oil of lemon eucalyptus (OLE), which is a much longer lasting and more effective mosquito repellent than the unprocessed oil.
In fact, OLE is the only mosquito repellent derived from a natural essential oil that’s registered with the EPA (Environmental Protection Agency) and that’s endorsed as safe and effective by the CDC (Centres for Disease Control and Prevention). It's one of the "big four" that we mentioned earlier.
OLE ranks right up there with conventional synthetic repellents like DEET and Picaradin, and with other highly rated “biopesticide repellents” like IR3535 and 2-undecanone.
#5 - Natural topical repellents
Many people prefer to use organic mosquito repellents to avoid the potentially adverse effects that synthetic repellents may have on their health, their children’s health and on the environment.
The good news is that repellents based on natural essential oils can be very effective against mosquitoes, some even more so than their synthetic counterparts.
The bad news is that compared to synthetic repellents, the effectiveness of essential oils tends to be short-lived because the constituents in them that deter mosquitoes are quick to evaporate from the skin.
But if you’re happy to keep re-applying the essential oil every 1-2 hours (more frequent applications are required if you're sweating or going in the water) then you can maintain pretty decent protection against mosquitoes and other bugs.
It’s very important to note that many essential oils are only effective as mosquito repellents when undiluted or weakly diluted.
Rather problematically though, some essential oils can cause skin irritation and dermatitis in certain people, especially when used at high concentrations.
Some undiluted or weakly diluted essential oils will also give off a very overpowering fragrance that certain people may be unable to tolerate.
For these reasons it’s usually best to use essential oils with a carrier oil (also known as a base oil) and you might also want to do a patch test on a small area of skin to see if you’re sensitive to a particular oil before applying it over a larger area of your body.
For oils that must be used at high concentrations to achieve good repellency, it may be a good idea to wash them off the skin soon after use.
Another thing to watch out for with essential oils is photosensitization, which is where the applied oil causes your skin to become more susceptible to UV rays and hence sunburn.
Photosensitizing agents are typically present in citrus oils like bitter orange, lemon, lime, tangerine, grapefruit and bergamot oils, although the effect can be somewhat negated by diluting the oil.
Essential oils can be bought online in their pure form and diluted with water or a carrier oil as desired. These homemade mosquito repellents can be applied topically or used in a spray bottle as a room spray.
Essential oils can also be blended with other essential oils to improve repellency. Commercial mosquito repellents are also available that are based on one or a combination of different essential oils.
What follows is a brief summary of the essential oils that have shown the most promise as mosquito repellents. It’s not an exhaustive list and there is still much more experimentation to be done in this field by scientists.
You should also experiment yourself and test other essential oils to see what works best for you. There are approximately 150 commercially important essential oils to begin experimenting with and in total there are over 3,000 essential oils known to mankind.
Eucalyptus oil

Considered to be one of the most effective natural mosquito repellents, eucalyptus oil is obtained by steam distillation of the leaves of certain species of eucalyptus.
Most of the world’s eucalyptus oil is produced from the Australian species, Eucalyptus globulus (Southern Blue Gum).
Even just heating Eucalyptus leaves will release certain volatile compounds into the air that will discourage mosquitoes from entering the space.
Try Artizen Eucalyptus Essential Oil (100% pure and undiluted).
Citronella oil

Citronella oil is extracted by steam distillation of the leaves and stems of a number of species in the Cymbopogon (lemongrass) genus, which is widespread throughout the tropics and sub-tropics.
Most of the world’s citronella oil is produced in China and Indonesia, though several other countries also contribute to global production.
There are two chemotypes of citronella oil; the Java type, (obtained from Cymbopogon winteranius) and the Ceylon type (from Cymbobogon nardus).
This essental oil has over 80 constituents, though the 3 most important ones are citronellal, geranial and limonene. Some studies have found it to be the most effective essential oil for repelling mosquitoes.
Try Organic Citronella Essential Oil (100% pure and undiluted) by Healing Solutions.
Similar to citronella oil is lemongrass oil, which comes from Cymbobogon citrata and has similar insect-repelling properties.
Confused about the difference between lemongrass and citronella?
One major difference between the two plants is that lemongrass is often used as a flavour-imparting herb in Asian cooking or in herbal teas, whereas citronella is not considered fit for human consumption.
Catnip (nepetalactone) oil

Nepetalactone oil is obtained by steam distillation of the leaves, stems and flowers of the European native herb Nepeta cataria (commonly known as catnip or catmint), which is a member of the mint family.
In a study carried out by Iowa State University research group researchers came to the conclusion that nepetalactone oil was ten times more effective than DEET at repelling mosquitoes.
Try Catnip Essential Oil (100% pure and undiluted) by Plant Therapy.
Peppermint oil

Peppermint oil is distilled from the leaves and flowers of the hybrid peppermint plant Mentha x piperata, a native of Europe and the Middle East that is a cross between Mentha aquatic (water mint) and Mentha spicata (spearmint).
This essential oil is a general insecticide and one study demonstrated that 100% of Culex quinquefasciatus mosquito larvae had died within 24 hours of being placed in water that a few mililitres of peppermint oil had been added to.
Try Cliganic Organic Peppermint Oil (100% pure and undiluted), which is certified by the USDA.
Cinnamon oil

The aromatic spice that most of us call cinnamon is simply the dried inner bark of various evergreen tree species in the genus Cinnamomum, which is found in Southeast Asia, China, Australia and even in Africa.
To prepare the spice, the larger sheets of cinnamon bark are dried and ground into cinnamon powder while bark peeled from the smaller twigs and shoots is kept whole, curling as it dries to become the familiar rolled sticks or quills of cinnamon.
Cinnamomum verum (Ceylon cinnamon) is the “true” cinnamon and most of it comes from trees grown in Sri Lanka.
C. verum is of a higher quality than Cinnamomum cassia (Chinese cinnamon), which is the cheaper, more strongly flavoured, most commonly consumed variety that dominates the supermarkets.
The majority of the world’s Cinnamomum cassia supply comes from Sumatra’s Kerinci valley, with the rest coming from China, Vietnam and Burma.
Cinnamon essential oil is usually extracted by cold-pressing or steam distillation of the bark and leaves of cinnamon trees, with the oil extracted from the bark usually being slightly costlier due to the greater difficulty involved in extraction.
One study conducted at the National Taiwan University found four compounds in cinnamon essential oil to be effective at killing the emerging larvae of the yellow fever mosquito, Aedes aegypti, although the oil was not tested on adult mosquitoes.
Try Organic Cassia Cinnamon Essential Oil (100% pure and undiluted) by Healing Solutions.
Clove oil

Clove oil is steam distilled from cloves, which are the dried, aromatic, unopened flower buds of Syzgium aromaticum, an evergreen tree in the Myrtle family that is native to the Maluku islands of Indonesia but which is now widely cultivated throughout the tropics.
Indonesia is the world’s largest producer of cloves and clove oil by far, with Madagascar and Tanzania trailing far behind.
In one study, clove oil was found to provide 100% protection against three species of mosquito for longer than the 38 other essential oils that were tested.
Try Artizen Clove Essential Oil (100% pure and undiluted).
Thyme oil

Another potent mosquito repellent, thyme oil is steam distilled from the leaves and flowers of Thymus vulgaris (common thyme) or Thymus zygis, two herbs that belong to the mint family and are native to Southern Europe.
The thyme oil produced in Spain or Turkey comes from T.zygis whereas that produced in France and other countries is derived from T.vulgaris.
One study that compared 5 different essential oils found thyme oil (along with clove oil) to be the most effective at repelling mosquitoes, providing 1.5 to 3.5 hours of protection depending on the concentration.
Try Thyme Essential Oil by Healing Solutions (100% pure and undiluted), which is thyme oil extracted from T.zygis. It comes in a Euro-dropper bottle for convenience.
Patchouli Oil

This essential oil is steam distilled from the dried leaves of Pogostemon cablin, a herb (belonging to the mint family) whose origin is shrouded in mystery, but is now cultivated widely throughout the tropics.
Although many countries produce patchouli oil, Indonesia is by far the world's greatest supplier, accounting for over 90% of global production.
In the previously mentioned study that compared the mosquito repellency of 38 essential oils, patchouli was one of the three oils that were deemed to be the most effective out of all 38 that were tested.
Try Artizen Patchouli Essential Oil (100% pure and undiluted).
Neem oil

Neem essential oil is extracted from the fruits and seed kernels of Azadirachta indica (neem tree), which is endemic to the Indian subcontinent but has since been introduced to other parts of the tropics.
Indian people have long known about the tree’s anti-fungal, anti-bacterial, anti-inflammatory and anti-aging properties.
The leaves of neem have been burned to ward off insects and the seed kernels contain an extremely potent growth-inhibiting compound called azadirachtin, which disrupts the feeding, growth and reproductive processes in many types of insects that are exposed to it.
Unfortunately, there’s a paucity of reliable studies on Neem essential oil as a mosquito repellent and experiments have shown mixed results.
However, one recent studythat was carried out in an Ethiopian village found Neem oil to provide 70% protection for 3 hours against the Anopheles arabiensis mosquito, the principal malaria vector in Ethiopia.
During the same study, DEET and MyggA (another commercially available repellent) were observed to have provided over 96% protection for an average time of 8 hours.
Try Milania Neem Oil. It’s organic, cold-pressed and 100% pure and undiluted.
#6 - Permethrin

Chemical formula: C21H20Cl2O3
Permethrin is a synthetic contact insecticide (belonging to the pyrethroid family) that was invented in 1972 by a British chemist named Michael Elliot.
Permethrin is a pyrethroid - pyrethroids are synthetic analogues of pyrethrins, a class of naturally occurring insecticidal organic compounds that are normally derived from the flowers of the Chrysanthemum plant, Chrysanthemum cinerariifolium.
Permethrin was one of the world’s first agriculturally viable insecticides and is still used in many countries to that end today, although it was banned for agricultural use in the EU in 2003. India is currently one of the world’s largest producers and exporters of the chemical.
Permethrin has a long history of use in the military and is still used to treat the uniforms and bed nets of soldiers of the British and US armies to give protection against mosquitoes, ticks, ants, mites and other biting insects. It is only since 2003 however that permethrin-treated clothing has been available to civilians.
Although permethrin can be used topically at high concentrations to treat scabies and head lice (usually sold over the counter under the names Nix and Elimite for this purpose), as a mosquito repellent it is never applied directly to the skin and is only used to treat clothing and other equipment.
Clothing (outerwear only, not underwear), shoes, backpacks, hats, mosquito head nets, bed nets, camping gear (tents, tarps, bivvy bags etc.) and other such items can all be impregnated with permethrin to make them repel mosquitoes and other insects.
In fact, clothing and gear that has been impregnated with permethrin will not only repel mosquitoes but may also kill or incapacitate them on contact, the latter effect being known as a “knock-down”.
Once properly treated with permethrin, clothing, gear and nets will retain their repellency even after going through the wash several times (you should hand wash or use a gentle cycle in the washing machine to help preserve effectiveness for longer).
So how does a traveller get his hands on this stuff?
Well, you can actually just go out and buy special outdoor clothing that has already been pre-treated with permethrin if you don’t want to do the treatment yourself.
This option has the advantage that the treatment will usually remain effective for much longer than the DIY method. For example, some companies claim that their permethrin-treated clothing can endure 70 washes before losing effectiveness.
Clothing and gear that you treat yourself on the other hand will probably need to be re-treated after about 6 washes, and once a month or so even if you don’t wash it at all.
The DIY method however means that you don't have to go out and buy a whole new set of permethrin-infused clothes, and you can just treat your regular travel wardrobe with a spray can.
Procedure for treating clothing with permethrin
If you want to impregnate your clothing and other gear with permethrin in the DIY fashion, the first step is to hang up your clothing and any other gear to be treated on hangers outdoors (never do this indoors), so that you minimize inhalation of the fumes from the spray.
It’s best to use permethrin that is approved for treating clothing, as this is formulated with certain ingredients that help it to adhere to fabrics. You can try Repel Permethrin Aerosol Spray, which is specially designed for treating clothing and gear.
The stuff that’s used as an agricultural insecticide might not stick to the fabric as well and you might also end up with the wrong concentration after diluting it if you don't know what you're doing, so it's better to stick to the dedicated aerosol spray.
Many people make the mistake of spraying everything too lightly – you need to be a bit heavy-handed, spraying the clothing and gear until it turns noticeably darker in colour and is thoroughly dampened (although it shouldn’t be dripping wet).
Once the process is complete, the treated clothing and gear should not be worn or used until it has fully dried.
It’s important to be aware that permethrin-treated clothing and gear alone will not provide adequate protection against mosquitoes and other insect pests.
Remember that permethrin is only applied to clothing, gear and nets, so it won’t protect any exposed skin that you may have on display.
For this reason, you should always use permethrin treatment in conjunction with a topical mosquito repellent that you apply directly. to your skin.
As regards the health implications of exposure to permethrin, it’s generally considered reasonably safe for humans when used in the correct fashion. However, you shouldn’t apply it to your bare skin, as it could cause irritation or even burning.
For fish and cats, permethrin is an entirely different story, as both animals are extremely susceptible to the stuff and can die when exposed to low levels of it, so don’t let it get anywhere near your fish bowl, aquarium and cats.
#7 - Clip-on mosquito repellents

Clip-on mosquito repellents are a type of spatial repellent that are designed to create a zone around your body that mosquitoes are discouraged from entering.
These gadgets are usually comprised of a compact, portable unit that incorporates a miniature fan and a replaceable cartridge that contains the active repellent ingredient, which is often metofluthrin or some other pyrethroid compound.
You can clip these gizmos onto your belt or pocket while you go about your business and the little battery-powered fan will blow and disperse the repellent into the space surrounding your body.
Manufacturers claim that their products can provide 8-12 hours of full-body protection from biting mosquitoes, but many consumers have reported receiving multiple bites while relying on these clip-on devices for protection.
Check out this video, which reports on an informal experiment that was carried out by Consumer Reports to test the efficacy of one of these clip-on repellents.
During the experiment, test subjects were kitted out from head to toe in protective gear (think beekeeper-type suit) and exposed to hundreds of bloodthirsty mosquitoes inside a screened enclosure.
The test subjects were monitored closely to see how many mosquitoes landed on their bodies and they were also asked to expose a portion of bare skin on their arms to see how many bites they received.
The purpose of the experiment was to verify one manufacturer’s claim that its product is effective for 8 hours but unfortunately, the experiment had to be curtailed after just 2 hours due to the test subject’s being repeatedly bitten by the hungry mosquitoes.
Consumer Reports ended up including clip-on repellents in an article entitled "5 Types of Insect Repellent to Skip".
In spite of the alleged outcome of the Consumer Reports experiment, some people do swear by clip-on repellents, so there probably are certain conditions under which they can be effective.
It’s likely that in situations where only a moderate level of protection is required, these gadgets could help to prevent biting. It’s logical that they would be most effective in windless conditions and when the user is remaining stationary.
If using the clip-on repellent while walking for example, the repellent would tend to trail behind you instead of forming a protective barrier around you.
Topical repellents are generally considered to be much more effective for outdoor use, but if you’ve experienced adverse side-effects or have had other issues with topical repellents in the past and you’re looking for alternatives, I would say there is no harm in giving these clip-on repellents a try.
You can check out Off! Clip-On Mosquito Repellent, which comes with included AAA batteries for the fan and one repellent refill. Additional refill packs can be bought separately. Each repellent disc is supposed to provide up to 12 hours of head-to-toe protection.
#6 - Mosquito repellent bracelets

Mosquito repellent bracelets are another kind of spatial repellent that have always been an enticing solution for the irresistibly attractive (to mosquitoes) traveller.
The notion that one can simply slip a stylish-looking bracelet over one’s wrist and suddenly have full immunity in all situations from mosquito bites has undeniable appeal; it recalls the magic talisman or amulet that many people wear for good luck and protection from evil powers.
Made from silicone and often adjustable to fit all sizes of wrists and ankles, mosquito repellent bracelets or wristbands are typically impregnated with natural essential oils like lavender oil or citronella oil, causing them to give off an odour that mosquitoes can’t stand.
If stored after each use in the original sealable pouch they come with, these fragrant bracelets can supposedly remain effective for up to 240 hours. They normally come in a wide selection colours and are even safe for infants to wear.
Some people will swear by the efficacy of mosquito repellent bracelets, whereas most experts will probably tell you that they are a total sham or that they only offer localized protection from bites in the wrist area where they are worn.
I personally would never trust them with my life if I was going into the jungle or trekking in other mosquito-plagued environments. But if your life is not at stake, then sure, there would be absolutely no harm in trying them out to see if they work for you.
A popular choice are the Mosquitno Waterproof Mosquito Repellent Wristbands, which are infused with natural citronella oil and are supposed to provide up to 5 days or 120 hours of protection.
The bands are lightweight, comfortable to wear and come in a range of colours (our favourites are the camo and tie-dye). After use they store in a resealable pouch to preserve their effectiveness.
#7 - Mosquito repellent patches

Mosquito repellent patches are fragrant, adhesive patches or stickers that are designed to be stuck to clothing, tables, bedsides, prams (if you have an infant) and so on, in order to ward off mosquitoes.
They are primarily marketed at children and families, as could be guessed from the cartoonish images that are displayed on the patches of many brands.
Mosquito repellent patches are usually impregnated with one or more 100% natural essential oils and are supposed to act as spatial repellents, creating an invisible mosquito net around you. Some products will claim to offer up to 72 hours of protection.
It's doubtful that these patches have a very strong effect on mosquitoes, but they are probably better than nothing. You can try these DEET-free Repellent Patches/Stickersby Mosquito Guard.
Keep reading to learn about more types of spatial repellents like camphor tablets, mosquito repellent candles and plug-in vaporizers, which we cover in the section below on how to keep mosquitoes away while at your hotel.
When you’re travelling, your accommodation is the one place that needs to be a refuge from mosquitoes and other biting insects.
You should be able to relax completely and not have to worry about contracting dangerous illnesses like malaria, dengue and chikungunya.
Unfortunately however, unless you’re willing to shut yourself inside an airtight, hermetically sealed box with no windows, gaps or air vents, a few mosquitoes will probably find their way into your room if your locality has a reasonably large population of them.
Insect mesh screens installed over the windows in some rooms can definitely help, but still can’t be relied on to keep the bugs out entirely.
Beach huts, stilt houses, humble rural cottages and other types of cheap accommodation can be especially prone to mosquitoes due to the rooms being less well sealed in general.
When mosquitoes do manage to infiltrate your private space, that presents a real problem, as they can seriously disrupt your sleep and your ability to relax, and you can’t simply walk away from the problem like you can often do in the outdoors.
Below we’ve outlined the best solutions for ensuring that the bugs stay out of your hotel room.
#1 - Stay in an eyrie

The word “eyrie” or “aerie” most commonly refers to an eagle’s nest built high in a tree, on a cliff ledge or in some other inaccessible location.
But the term can also refer more generally to any relatively high or inaccessible place from which one can observe everything below them.
In this context, we’re referring to a hotel room that’s situated high up in a tall building. By elevating yourself to lofty heights, you remain far removed from the insect-related problems and concerns that afflict the ground dwellers below.
This works because mosquitoes generally don’t like to stray more than 50-100 metres, either horizontally or vertically, from their breeding grounds.
In the case of really tall buildings there will also be a noticeable drop in air temperature and an increase in wind velocity as you go higher, both of which discourage mosquitoes.
This doesn’t mean that you won’t ever find mosquitoes flying near the tops of tall buildings (you will) but it means that the probability of encountering them decreases as you ascend higher.
How high do you need to go to see a difference? It’s generally recommended that you choose a room on the 4th floor or higher.
Rooms that are really high up are often associated with luxury hotels but occasionally you can snag eyries at budget prices.
In a past trip to Manila, Philippines, we stayed in a Zen Rooms Space Taft budget room on the 27th floor of a skyscraper.
The room had free Wi-Fi, AC, ensuite bathroom, hot water, a fridge, a microwave, a large kitchen sink, free towels and a stunning view of the city below from the window, all for less than $10 a night. Needless to say, we had no problems with mosquitoes in that room.
#2 - Turn up the fan speed

It almost sounds like too simple a measure to be effective, but if you’re staying in a room with a ceiling, pedestal, table or wall-mounted fan, the air current it blows across your body can sometimes be all that’s required to keep hungry mosquitoes at bay.
But what if it’s cold and you don’t want to turn on the fan? Luckily, mosquitoes will mostly only be a nuisance when its warm, which is when you’d be turning on the fan to keep cool anyway.
A fan helps to keep mosquitoes away because:
(a) mosquitoes are unskilled pilots in high winds
(b) a fan helps to disperse the carbon dioxide, body odours and other chemical cues that allow mosquitoes to detect your presence and determine your exact location
While the really desperate or hungry mosquitoes will still try (sometimes successfully) to land on your alluring body in spite of the gale force winds, a fan running on its medium or high speed setting definitely helps to hold them off.
#3 - Turn on the AC

Just like with a fan, the air current generated by an AC unit makes it more difficult for mosquitoes to fly and also helps to disperse the odours that allow mosquitoes to pinpoint your location.
But the primary reason that air-conditioning can be so effective in banishing mosquitoes is because it lowers the room temperature and relative humidity to a level that mosquitoes don’t like. They hence become inactive and stop feeding.
Having the AC turned on will also mean that you cool down, which will cause you to emit less body heat and body odours (by perspiring less), which makes you less “visible” to mosquitoes.
Another thing to consider is that rooms that have AC installed tend to be more airtight, since the owner of the property will want to minimize his electricity bill. A more airtight room means fewer ways for mosquitoes to enter in the first place.
#4 - Exterminate the existing intruders, then prevent any new ones from re-entering

Want to completely purge your room of mosquitoes and then make sure that no new ones enter?
Mosquitoes aren’t that difficult to dispatch, especially if there are only a few of them lurking inside the room.
One tactic that can work well is to lie motionless on the bed for a few minutes with the fan turned off, waiting patiently for any mosquitoes to land on you.
Then when a mosquito makes contact with your skin, decides the coast is clear and begins to feed on your blood, you can then suddenly, with a lightning-fast motion of the hand, splat it against your body.
Mosquitoes are also easy to spot and splat when they’re perched motionless on the wall (although this does often leave behind a bloody mess), especially if the wall is painted a light colour like white or cream.
For airborne mosquitoes, you can crush them or capture them by making a tight fist around them with a rapid thrust of the hand.
Another popular means of dealing death is to clap both your hands together at just the right moment so that the airborne mosquito gets mashed in between them.
If for some reason the act of killing mosquitoes makes you feel guilty, you can also try to trap the mosquito in a glass or mug when it's sitting on a wall, table or other surface. You can then slide a piece of card or paper under the mug and transfer the mosquito to the outdoors.
Mosquitoes often like to skulk among potted plants, curtains, towels, hanging clothes and in other shady areas so make sure you inspect all these potential hiding places before concluding that you’ve eradicated them all.
Once you think you’ve exterminated all the mosquitoes in the room, you should then try to block off any gaps and openings from where they could potentially re-enter.
Close any open windows (you can leave them open if they have hole-free insect mesh screens), maybe try stuffing a towel underneath the door and try to block up any other obvious gaps that you can see.
Unfortunately, some rooms will have large ventilation openings (which may be fitted with metal security bars) at the top of the walls and these can be difficult to block up. If you ever find yourself in that situation, you should look at some of the other solutions.
#5 - Use an electric fly swatter to zap the mosquitoes
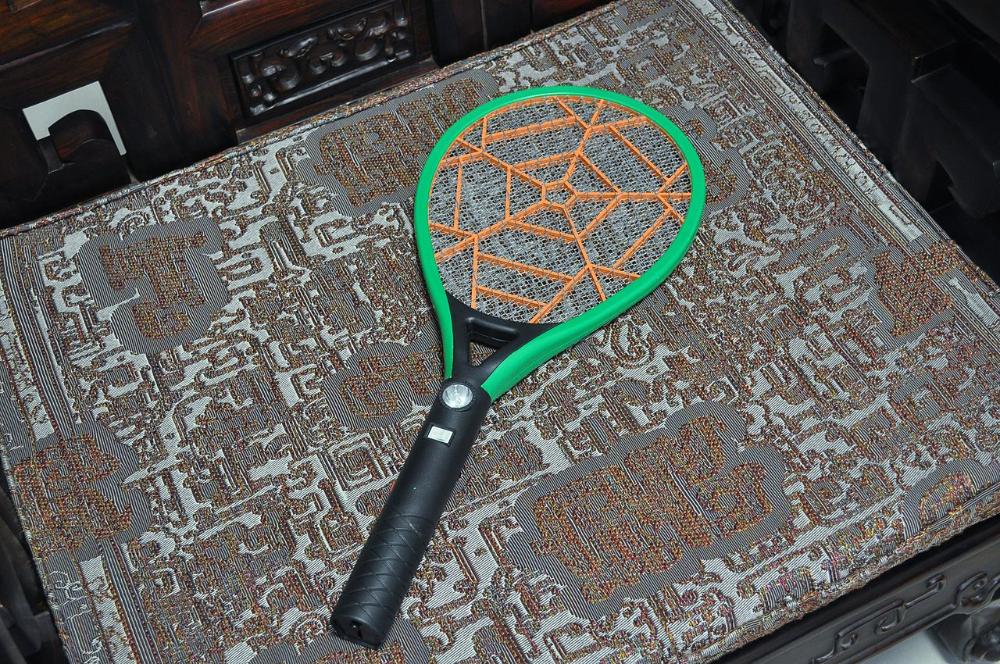
Electric fly swatters, also known as mosquito bats or racket zappers, are way too big and heavy to carry with you when travelling, but the owner of your hotel or guest house might let you borrow one to zap all the mosquitoes in your room.
These tennis-racquet-resembling contraptions run on rechargeable or disposable batteries and can generate very high voltages (usually 500 – 2,750 V) when a button on the handle is pressed.
Any mosquitoes (or other flying insects) that are unfortunate enough to fly into the metal grid of the racquet will die a spectacular death by electrocution, generating sparks, smoke and sounds like those of firecrackers going off in the process.
Many electric fly swatters possess a three-layer grid, which is comprised of an inner wire mesh layer sandwiched between two outer layers of parallel metal rods.
The inner mesh layer and outer rods are oppositely charged, so that when a mosquito touches against both simultaneously, a short circuit develops and a spark passes through the insect, stunning or killing it on the spot.
Another electric fly swatter design uses just a single-layer of parallel rods, with adjacent rods carrying opposite charges.
Regardless of the method of electrocution used, these contraptions are very effective at killing mosquitoes and other flies because their relatively open grid means that insects aren’t forewarned of their imminent death by a whoosh of air, as with traditional fly swatters.
Their other advantage is that they don’t require mosquitoes to be crushed against a wall, table or other flat surface, which usually leaves a terrible mess, especially when the mosquito is already filled with blood from a previous feeding session.
#6 - Camphor tablets

Chemical formula: C10H17O
Camphor is an age-old, natural mosquito repellent that people have used for generations to keep their living spaces mosquito free.
This white, volatile, aromatic, waxy, crystalline substance (a terpenoid ketone) used to be primarily made by distilling the bark and wood of the camphor laurel tree (Cinnamomum camphora), a native of China, Japan, Taiwan and other east Asian countries. Nowadays however, camphor is mostly synthesized from turpentine.
Camphor was used to make mothballs in the past, though these days mothballs are normally made from either naphthalene (a white solid derived from coal tar) or pdichlorobenzene.
The latter is probably best known for its use in those deodorizer cakes found in men’s urinals and it represents less of a fire hazard than naphthalene.
Camphor has also been used in toolboxes as the vapour it emits inhibits rust and you will find it as an ingredient in some cough medicines and in Vicks Inhaler nasal sticks too, as it works as a cough suppressant and decongestant. It also has anti-bacterial, anti-fungal and anti-inflammatory properties.
When you’re travelling you may come across shops that sell packets of small white camphor tablets or cubes.
If you want to expel mosquitoes from your room in a hurry, you can place one of these camphor pieces in a metal bowl or other non-flammable container and set it alight with a match or lighter.
Camphor tablets are highly combustible and when burned will fill the room with an acrid smoke that will drive any mosquitoes out, although there is always the risk when doing this that the fumes might drive you out of the room too.
A more gentle, slow-release approach is to just leave a few camphor tablets in the corners of the room and take advantage of the fact that camphor sublimes (turns directly from a solid into a gas without becoming a liquid) at room temperature. Within the day or so the tablets will have vanished.
Another common method is to place a few camphor tablets in a shallow ceramic or metal bowl that is suspended over a burning tealight.
The heat from the burning candle helps to vaporize the camphor more quickly, thus helping to ward off stubborn mosquitoes. The tablets could also be placed on other warm surfaces to achieve a similar effect.
Although camphor is highly toxic when ingested (just 5 g can be lethal to an adult human), the relatively modest amounts of vapour released into the room when using the gentler methods described above shouldn’t do you any harm when inhaled.
#7 - Mosquito repellent candles

Many people pack a small candle or a few tea lights when they travel to serve a variety of purposes including:
- Emergency lighting backup during unexpected power outages
- Relaxation or meditation at the end of a tiring day of sightseeing
- To create a romantic or homely ambience in the bedroom or bathroom
- To deodorize a fetid bedroom or bathroom
- To help create a bug and mosquito free environment.
For the lattermost purpose, ordinary candles won’t cut it - you’ll get far better results by burning a specially made mosquito repellent candle.
Mosquito repellent candles can vary in size from small tealights to much bigger candles and most are infused with or more plant-derived essential oils such as rosemary, peppermint, mint, tea tree, citronella, cedarwood, lemongrass and so on.
Most of these candles will produce a very pleasant aroma when burned due to the natural oils they contain.
It’s important to understand that mosquito repellent candles are not very potent deterrents and should not be relied on in travel situations where you might be liable to experience a severe mosquito onslaught.
Nevertheless, they can make a lot of sense when you’re planning to bring candles on a trip anyway, or if you aren’t expecting to have too much trouble with mosquitoes.
One of the upsides of mosquito repellent candles is that the vapours they give off are safer to breathe in than those of synthetic chemical repellents. The only significant risk with using these candles seems to be that certain people can be allergic to citronella.
I feel that the tealight-sized mosquito repellent candles are the most suitable for travel due to their compactness and portability.
Having a dozen or so tealight candles also allows you to light a ring of them around you so that you are encapsulated inside an invisible mosquito net. Tealights are usually designed to burn for 2-3 hours, which should be long enough to drive out the bugs.
You can try these fragrant Mosquito Repellent Tea Lights by Mosquito Guard, which come in a 16-pack. They're made with all-natural essential oils like citronella, peppermint, lemongrass, rosemary and cedarwood.
#8 - Use a mosquito net over your bed

Mosquito bed nets come in a variety of colours, sizes and shapes, including cones, pyramids, cylinders, domes and most commonly, boxes.
Whatever the design though, all serve the same purpose - to create a bug-free zone over your bed so that you can sleep without being tormented by mosquitoes.
As long as you remain inside this tranquil haven, mosquitoes can only buzz around outside the net in futility, being too big to pass through the fine mesh of the net to reach you. You'll still often hear the annoying high-pitched whine, but at least they won't be able to get you.
The only two caveats for the net to work properly are that the mosquito net shouldn't have any holes in it and your body shouldn't make contact with any part of the net while you sleep, as mosquitoes can then bite you through the net.
If everything is set up correctly, the mosquito bed net is an effective way to achieve a night of restful sleep in a room that’s teeming with famished mosquitoes.
The advantage of a bed net over some other methods (see below) is that you’re not inhaling smoke from incense or mosquito coils, nor are you breathing in potentially harmful chemical vapours from plug-in repellents.
However, bed nets also have a few drawbacks and some people don’t like sleeping under them for those reasons.
Firstly, they won't always be set up when you need them to be and the task of setting them up can be a bit of a pain if you're not familiar with the net design and the procedure. You might need to seek some assistance from a member of staff or the owner of your accommodation.
Secondly, bed nets make it a little inconvenient to get in and out of the bed during the night, like when you get up to go to the bathroom.
Each time you want to get out of bed the net will need to be untucked from underneath the mattress to allow you to exit, and will need to be re-tucked when you get back into bed.
Bed nets can also engender a sense of confinement, making you feel as if you’ve walled yourself inside a prison in order to keep the mosquitoes out.
If it's a warm night and you’re relying on a fan to stay cool, another issue with bed nets is that they can significantly hamper the airflow reaching you from the fan.
Sometimes you can compensate for this effect by just maxing out the fan speed, but what about those really warm nights when you need the full, unimpeded flow of air from the fan on the highest speed setting just to stay cool?
Another problem that can crop up, as we already alluded to, is that the mosquito box nets that you are provided with may be pockmarked with hole and tears (some of which may have been made by the red hot ends of cigarettes and joints that were carelessly smoked too close to the net by previous guests).
We have managed to patch up small holes in mosquito box nets in the past using electrical tape, which is why we usually carry a small roll with us whenever we’re on the road.
So, should you carry a mosquito bed net with you when travelling to countries where mosquitoes are rife?
Actually, I wouldn’t recommend carrying one for a couple of reasons.
The first reason is that in some rooms you may not be able to find viable attachment points that would allow you to suspend the net over the bed. In that very common situation your net becomes redundant.
The second reason is that in accommodation where mosquitoes are a major problem, the management will most likely be able to provide you with a bed net or will have some other solution for dealing with the mosquitoes.
#9 - Plug-in vaporizer mosquito repellents

Another solution for combatting mosquitoes in your room is an electrical device known as a plug-in vaporizer, which diffuses chemical vapours that are hazardous to mosquitoes (and relatively harmless to humans) throughout the room.
Plug-in vaporizers fall under the category of spatial repellents, as opposed to topical repellents that you would apply directly to your skin.
(There is another plug-in device that uses ultrasonic waves to ward off mosquitoes, but we are not recommending these here, as they have been largely dismissed as being ineffective by the scientific community.
If you're still interested you can check out the Neatmaster Ultrasonic Pest Repeller, which claims to be effective against a whole host of pests including bed bugs, mosquitoes, spiders, ants, flies, cockroaches, fleas, mice and more. The device lets you choose between three different modes, depending on the severity of the infestation. Surprisingly, the product has a lot of glowing reviews on Amazon.)
I am not sure if plug-in repellents are used in all the world’s mosquito-plagued countries, but I do know that in India they are quite commonly used in households, with Good Knight, All Out and Mortein being among the best-known brands there.
The “Good Knight” brand of plug-in vaporizer that I’m familiar with resembles a bulky adapter. It consists of an electric heating element enclosed within a hard plastic casing. Into the unit screws a small, replaceable, 45 ml PET bottle that is filled with a colourless, volatile liquid mixture.
Assuming typical daily use (7-8 hours), a single one of these replaceable bottles will usually last for about 3 weeks and, in India at least, they cost about €1 or Rs. 80/- each to replace. That works out at about €0.04 for a full night of mosquito protection.
The active ingredient in the liquid mixture is usually some kind of pyrethroid insecticide like allethrin, prallethrin, transfluthrin etc. at a low concentration of 1.6% w/w.
As we mentioned previously, pyrethroids are synthetic compounds that mimic pyrethrum, a natural insecticide found in Chrysanthemum flowers.
They are a popular choice in mosquito repellents because at low concentrations they are highly toxic to insects but relatively harmless to mammals (including us humans).
The other crucial component in this technology is the porous clay carbon wicking rod that passes through a hole in the top of the bottle so that the bottom of the rod is immersed in the liquid and the top sticks out of the bottle.
When the device is plugged into a working power outlet, a small indicator light will come on to indicate that it’s now active. A switch on the unit allows you to toggle between “Activ+” and “Normal” modes, depending on how pesky the mosquitoes are.
When switched on, the liquid inside the bottle is continuously being wicked up to the exposed top part of the clay carbon rod via capillary action, where it gets vaporized by the heat from the electrical heater.
The vapours immediately begin to diffuse through the room and start to work their intoxicating magic on the mosquitoes. After about 9 minutes it should supposedly start having an effect, but in my experience it can sometimes take a bit longer than that for the biting to abate.
The active ingredient in the vapour disrupts the nervous system of the mosquitoes, causing them to lose control of their bodily movements (ataxia). They soon become flightless (an effect known as KD or knock-down) and paralyzed.
Any mosquitoes outside the room are also deterred from entering while the vaporizer is plugged in, as they essentially see it as a hostile environment.
One of the primary advantages of plug-in vaporizers is their ease of use. The only preparation required is to ensure that all windows and doors are closed and then it’s really just a matter of plug and play.
As long as you don’t have any protracted power outages during the night, any mosquitoes that were in the room should remain knocked out until the morning.
Keeping a fan running in the room while the vaporizer is switched on is not a problem and will help to disperse the active ingredient throughout the space more rapidly.
Plug-in vaporizers are preferable to mosquito coils (see below), which can require fiddling around with matches for several minutes to get them lit, can require relighting during the night and which fill the room with noxious smoke, which is definitely not good to be breathing in!
It’s worth noting however that not all mosquitoes are equally affected by pyrethroid vapours, with differences observed between species and also individuals. Some strains have even become resistant to certain pyrethroids.
Bear in mind also that these plug-in vaporizers are designed to be used in smaller rooms and will become less effective in very commodious rooms, as the poisonous vapours will become too dispersed.
In general though, these plug-in vaporizer repellents are effective and they get the job done.
As regards safety for humans, although many people can leave a vaporizer plugged in all night without suffering any ill effects, some people do report headaches and people with asthma can be particularly sensitive.
Cats are also particularly vulnerable to pyrethroids (due to an inability to metabolize them efficiently), so if you travel with a pet cat, this is not the right mosquito-repellent solution for you.
To minimize your exposure to the vapour, it’s recommended that vaporizers be plugged into the power outlet that’s furthest away from where you’re sitting or sleeping in the room.
So, should you carry a plug-in vaporizer with you on the road?
Plug-in vaporizers are lightweight and fairly compact, and you can’t always count on your hotel or guesthouse to be able to provide one, which is why some people carry one at all times during their travels.
If you’re on the move with a vaporizer, always remember to unscrew the bottle from the main unit and replace the original screw cap that came with the bottle to prevent spillage of any liquid.
Some people have suggested that both the liquid bottles and the electrical units should be placed in checked luggage, as some travellers trying to bring them in hand luggage have had them confiscated by airport security.
Also, it's worth noting that good quality heaters are usually serviceable for 3-4 years before needing replacement, whereas it’s recommended that you replace lower quality heaters every year.
In countries where the replaceable liquid bottles can be bought, you’ll normally find them for sale in convenience stores, mini-marts, general stores and the like.
#10 - Mosquito coils

Mosquito coils are spiral-shaped strips of self-combusting material that slowly burn like a fuse once lit, releasing a steady stream of smoke and mosquito-repelling vapour into the air.
Coils are widely used for mosquito protection throughout Asia, Africa and South America, but Europeans and North Americans will be less familiar with them, as they never became fashionable on these two continents for some reason.
The mosquito coil was invented in the late 1800s by a Japanese mandarin exporter named Eiichiro Ueyama, who was trying to create insect-repelling incense sticks from a starch base mixed with dried, powdered Chrysanthemum flowers, which contain the natural insecticide pyrethrum.
Ueyam's wife suggested that he could make the sticks burn for longer by making them longer and coiling them into a spiral, thus giving birth to the first mosquito coil. The coils proved to be a hit and were hand-rolled until the process was mechanized in 1957.
Nowadays mosquito coils come in a variety of different colours and sizes, and are designed for both indoor and outdoor use.
The active ingredient in the coils of today is usually some kind of pyrethroid (synthetic insecticide) like prallethrin, d-trans allethrin, or some type of natural essential oil.
The combustible base material is normally made from biomass and is infused with a very small amount of the active ingredient (typically 0.04% - 0.1% w/w).
Mosquito coils usually come with a small upright metal stand, which has a sharp point that can be pushed into the centre of the coil so that it is supported a few inches above the ground and doesn’t leave scorch marks on the floor as it burns.
Once lit a typical mosquito coil will burn continuously for around 6-8 hours, although I have also come across larger coils that will burn for 12 hours.
Occasionally, burning coils can get extinguished for no apparent reason and have to be relit again. If there is a lot of air circulation from say, a breeze or a fan, coils will burn faster and won’t last as long, although they are less likely to go out prematurely.
Mosquito coils are usually comparable in cost or even slightly cheaper than plug-in repellents. In India for example, a box of 10 standard size coils costs just Rs. 26/-, which works out at about €0.03 per coil providing 6-8 hours of protection.
Coils (and bed nets) are commonly used in low-income households in tropical and sub-tropical countries, since they are cost-effective and also not reliant on electricity like the plug-in repellents.
Personally, I’m not a big fan of burning mosquito coils in confined, indoor spaces because the smoke from them irritates my eyes, causing a burning sensation accompanied by profuse waterworks.
For some people, the smoke can also irritate the lungs and throat. It’s plausible that long-term exposure to the particulate matter from burning mosquito coils could lead to lung problems, though infrequent use is probably not too hazardous.
It is possible to reduce the amount of smoke you’re exposed to when burning mosquito coils by placing the burning coil further away from where you’re sitting or sleeping, by keeping windows and doors open and also by only burning coils in large, airy rooms.
Another option to reduce inhalation of smoke is to “fumigate” the room by vacating it for a few minutes while the burning coil fills the room with smoke and drives out all the mosquitoes and other bugs.
You can then extinguish the coil and wait for the smoke to be mostly cleared before returning to the room and then blocking off any gaps that mosquitoes might re-enter from.
If you're travelling to a place where you might not be able to buy mosquito coils locally, you can also buy them online before your trip. Try these S C Johnson Off! Mosquito Coils, which come in packs of 6 and burn for 4 hours each with a country fresh scent.
#11 - Incense

When you hear the word “incense”, it probably conjures up images of combustible cones or coated sticks that are burned to suffuse a room with a pleasant fragrance or to help with meditation or relaxation.
Incense has been used in various parts of the world since antiquity as an aid in ritual, meditation and healing. It has also been used as a simple air freshener and as an insectifuge (insect repellent), which is the use we’re most interested in here.
When incense is burned it produces a continuous stream of smoke that slowly diffuses through the surroundings, thus helping to drive away mosquitoes and other insects.
Regular incense sticks usually burn for 20-30 minutes, while other forms of incense can burn for much longer.
Today much of the world’s incense is produced in India, where around 200,000 local women work part-time in hand-rolling raw, unscented incense sticks at home.
The incense sticks are produced by adding water to a blend of dry, powdered ingredients to form a moldable paste or dough, which is rolled onto a thin stick and then left to dry over a period of several days to form the semi-finished product.
The rolled sticks are then passed on to any of the country’s (roughly) 5,000 incense companies, which apply their own unique brand of perfume and then package the incense sticks for sale.
The price per stick can vary depending the brand and ingredients used, but I’ve seen boxes of 90 incense sticks sell for just 29 rupees in India, which pegs the price per stick at less than half a (US) cents, making incense a pretty cost-effective mosquito repellent.
But is incense actually an effective mosquito repellent? Will it keep mosquitoes out of your room? It’s probably true that burning incense is in most cases not as effective as burning say, a mosquito coil.
Regular incense sticks produce a smaller quantity of smoke than a coil and their primary function is to fill the room with a pleasant fragrance, not to fill it with smoke and drive out mosquitoes. Incense cones however produce a greater quantity of smoke than the sticks and should be more effective.
I would say that if you’re staying in a relatively small room and mosquitoes are not bothering you that much, burning two or three incense sticks might be all that’s needed to keep them at bay.
I often burn incense myself when I’m getting the occasional mosquito bite and I do find that it makes a difference.
When you’re travelling and mosquitoes strike, we recommend buying a pack of the self-combusting, masala-style Indian incense sticks, which are known in India as agarbatti. Once ignited, you can just leave them alone to slowly fill the room with their smoke and fragrance.
There are other kinds of incense that are not self-combusting and instead require an external heat source such as a burning piece of charcoal or an electric incense heater, but when travelling it’s best to stick with the self-combusting forms, since these are the simplest.
Because incense-making is a highly unregulated industry, we also advise that you try to stick to natural incense made from all-natural powdered ingredients like roots, stems, leaves, flowers, fruits, wood, gums, resins, essential oils and so on.
Some of the common natural ingredients used in making incense include sandalwood, cedar wood, star anise, patchouli, turmeric, clove and ginger.
The type of incense to avoid is synthetic incense (also known as dipped incense), which is made by dipping blanks, which have been shaped into sticks or cones, into fragrant synthetic oils to scent them.
The problem is that many of these fragrant oils, while perfectly safe when used as intended, are not meant to be burned, and doing so may release harmful fumes into the air.
Some manufacturers will also add extenders like dipropylene glycol (DPG) to these fragrant oils in order to dilute them and increase profits. The problem with DPG is that it releases poisonous gas into the air when burned!
Even the blanks that are used in synthetic incense can be problematic, as they are sometimes made with sawdust from plywood, which contains toxic glues that can release formaldehyde when burned.
With synthetic incense, there’s just no way to know what you’re really burning, which is why it’s best avoided.

The word “mosquito” actually derives from the Spanish mosca (fly) and the suffix ito (small), so it literally means “little fly”.
Mosquitoes are small, flying, six-legged insects belonging to the family Culicidae, which is within the order Diptera (the true, two-winged flies).
They have a pair of compound eyes, a pair of antennae (which are noticeably bushier in males compared to females), a pair of wings, a slender segmented body, three pairs of legs and very sophisticated mouthparts for siphoning blood from their victims.
Some interesting facts about mosquitoes are that they can beat their wings between 450 and 600 times per second and their abdomens can hold three times their own weight in blood.
Mosquitoes have existed in one form or another for at least 90 million years, as is evidenced by the find of a partially preserved adult female mosquito (Burmaculex antiquus) in Burmese amber that has been dated at 90-100 million years old. The mosquito belongs to Chaoboridae or the Jurassic fossils, a sister group of Culicidae.
A one-of-a-kind rock fossil of a 46-million year old, blood-engorged mosquito was even discovered by amateur fossil hunters in Montana over three decades ago.
There are 112 genera and over 3,500 species of mosquitoes in the world at present and the bloodsucking nuisances are found on every major landmass except for Antarctica.
With that said, there is one island that is believed to be completely mosquito-free and that is Iceland.
The absence of mosquitoes in Iceland is an intriguing mystery and it’s still not clearly understood why this small European island amid the North Atlantic doesn’t support them.
Temperatures in Iceland are high enough for mosquitoes to thrive (as they do in Iceland’s neighbours like Norway, Greenland and Scotland) and there are plenty of ponds and lakes for them to happily breed.
Exceptions aside though, in most parts of the world mosquitoes are an ever-present menace that most of us have had to learn how to live with.
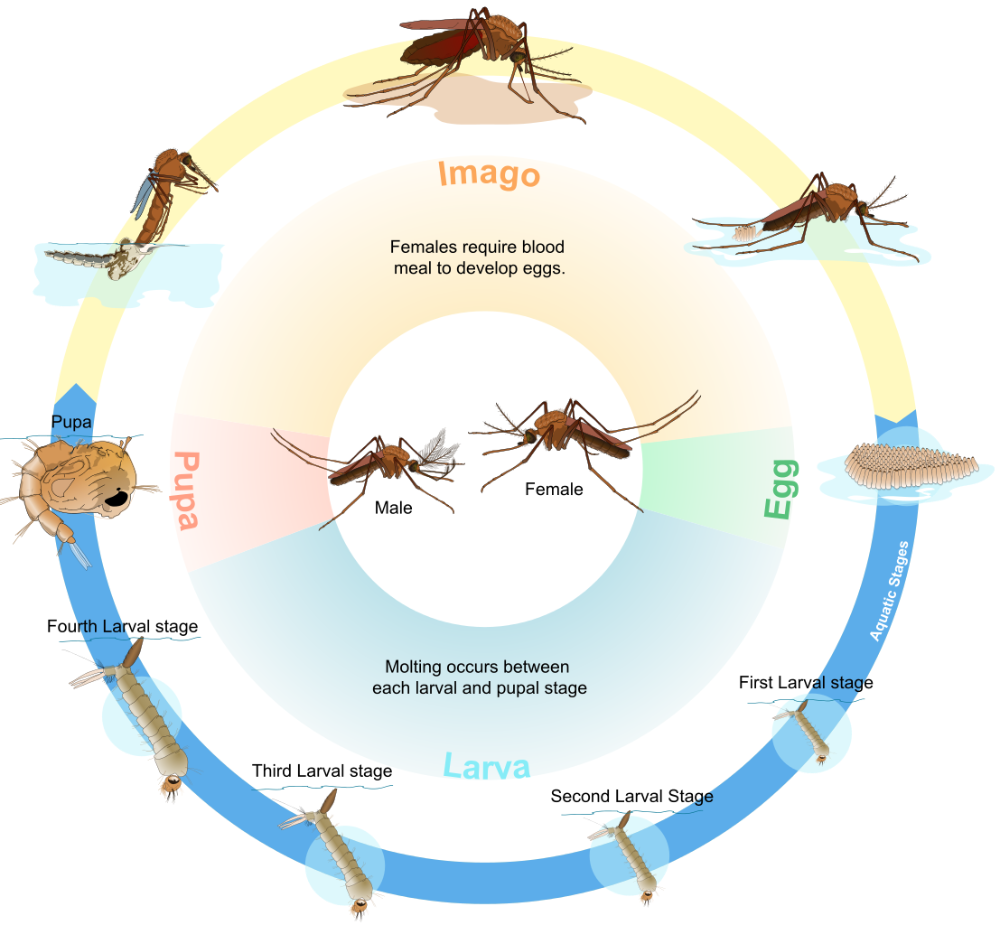
Mosquitoes have a four-stage life cycle, changing from egg to larva to pupa to adult (imago).
The cycle begins when a female adult mosquito lays a clutch of 100-200 eggs after mating and feeding on animal blood.
Depending on the species, the eggs might be laid directly on the water surface, in damp mud near the waterline or may be attached to the underside of water lily pads. Some species deliberately lay their eggs on the water surface in cohesive floating layers called rafts.
Note that mosquitoes don’t require a large water body like a pond or lake to deposit their eggs; even a miniscule puddle of water will suffice for many species. Some types of mosquito will lay their eggs in pitcher plants, hollowed out trees or cupped leaves that hold water.
In man-made environments, mosquitoes will lay their eggs where water has collected or where water might soon collect in a flower pot, old tyre, bird bath, blocked gutter, wheelbarrow, water butt, garbage can, children’s toy, pet water bowl hollow tree stump in the garden etc.
If the eggs survive desiccation, they will usually hatch within 1-3 days after being covered with water, although it could potentially take months for this to happen if the eggs are laid during the dry season or during a cold winter.
When the eggs hatch, the mosquito larvae emerge. They are capable of swimming and are often called “wigglers” or “wrigglers” due to the way that they move in the water.
The larvae develop by feeding at the water surface on algae, microbes and other organic material that they ingest via their mouth brushes.
Over a period of 7-10 days, each larva progresses through four stages of development known as instars, molting at the end of each stage, before it metamorphoses into a pupa.
The pupa is normally comma-shaped and it doesn’t feed but rather spends most of its time near the water surface so that it can breathe through its respiratory trumpets.
If the pupa senses danger, it can swim downwards to escape from the threat. The pupa is often called a “tumbler” because of the way it swims by flipping its abdomen. The pupa develops for 1-3 days until its casing splits and the adult mosquito emerges.
The adult mosquito can live for anywhere from a week to several months depending on the species, sex and weather conditions. In the wild most adults expire within two weeks, although in captivity they might live for a month or longer.
Some adult mosquitoes can extend their lifespans up to several months by spending the cold winter in diapause (a period of suspended development), only to resume activity again in spring when temperatures rise.
The adult mosquito typically begins to breed within a day or two of emerging from the pupal stage. With such a short life ahead, there’s no time to waste.
The female only has to mate once to be able to lay eggs throughout her life, though in the species that practice unautogenous reproduction she must also obtain a blood meal before she can produce any eggs.
Mosquitoes that practice autogenous reproduction on the other hand don't require a blood meal to lay eggs.
Some species may also be partially unautogenous, which means that they don't require a blood meal for their first clutch of eggs but do require blood to produce subsequent clutches.
After her blood meal the female will normally rest for a few days in order to digest the meal and develop her eggs.
The first clutch is normally the largest, with subsequent clutches being smaller, though a female will typically have multiple clutches throughout her life.
After each laying each clutch of eggs, the female will go off again in search of the next blood meal until she eventually expires.

You might think that the answer to this question is simply “animal blood” but the truth is that many kinds of mosquitoes never consume any blood at all.
Adult female mosquitoes in the genus Toxorhynchites, for example, don't require animal blood because their larvae prey on the protein-and-fat-rich larvae of other mosquitoes and these nutrients are passed onto the adults for egg production (oogenesis).
Even among hematophagous (blood-feeding) mosquitoes, both adult sexes primarily feed on nectar, plant juices and honeydew (a sweet, sticky substance secreted by aphids and deposited on leaves and stems of plants). These sugary fluids are stored in the crop and are released into the mosquito's stomach when needed.
But when it comes to the task of producing eggs the female in many species additionally requires a helping of animal blood (for the proteins and lipids it contains) after mating. Hence it is only the female mosquitoes that feast on your blood.
Recent research suggests that female mosquitoes can also become ravenous for blood when they are dehydrated, so it’s not always a matter of needing it to produce eggs.
In dry conditions where mosquitoes have limited access to water, a blood meal may serve as a thirst-quenching beverage on a hot day, which may explain why the rate of transmission of mosquito-borne illnesses can sometimes be higher during droughts.
One interesting thing to note is that feeding on blood decreases the lifespan of female mosquitoes considerably, and it's believed that they can live for several weeks longer if they only feed on sugary plant juices like nectar and tree sap.
When female mosquitoes go looking for a blood meal, they're usually quite selective about the source when they can afford to be. Most, if not all types of mosquito have their preferred hosts, which vary from species to species.
Some will target birds, monkeys, reptiles (including snakes), amphibians, livestock and even types of fish that expose themselves above the water (e.g mudskippers).
Remarkably few of the 3,000 or so known species of mosquitoes specialize in feeding on the blood of humans.
Despite their feeding preferences, most types of mosquito are also very adaptable, and will become more opportunistic feeders when their preferred host becomes scarce or unavailable.

Knowing when and where mosquitoes are likely to be most active can help you plan your trip better so that you can better avoid them.
When
Mosquitoes are normally active year-round in hot, humid tropical and sub-tropical countries, and this is why mosquito repellent and anti-malarial medication is the first thing that many people will think of bringing when planning a trip to the tropics.
Such parts of the world typically have a wet or rainy season, when mosquito numbers will often swell due to a profusion of puddles and standing water suddenly becoming available for egg-laying.
But it’s important to be aware that in colder parts of the world mosquitoes can also become highly active during the warmer months of the year, a period that is often referred to as the “mosquito season”.
Many people are not aware that mosquitoes can be very troublesome during the late spring, summer and autumn months in relatively cold Scandinavian countries like Norway, Sweden and Finland, especially as you go inland and further north.
It's not really the time of year that governs the activity level of mosquitoes, but the air temperature, with 10°C (50°F) being the threshold temperature at which mosquitoes will come out of hibernation or diapause and start to become active.
Mosquitoes are not very comfortable in lower temperatures however, and really only begin to thrive when the temperature is 27°C (80°F).
The reason mosquitoes are so strongly influenced by the outside temperature is because they are cold-blooded insects, incapable of regulating their own body temperature.
As well as the broader, seasonal variations in mosquito activity, there are also variations in activity levels according to the time of day.
Although some species will do the majority of their feeding during the day and rest at night, most types of mosquito will feed most actively at dawn and dusk, and may also feed during the night for several hours.
Two species that buck the trend and primarily feed during the day are the Asian Tiger Mosquito (Aedes albopictus) and Aedes aegypti, the species that is best known for propagating Dengue.
The Asian Tiger Mosquito is no saint either, and can transmit diseases like Zika virus, Dengue, West Nile Virus and Chikungunya.
Many travellers will be familiar with Aedes albopictus as the small, black-and-white-striped mosquitoes that bite in the shade of trees during the day.
The bottom line is that depending on where you are and what you’re doing, you might need to watch out for biting mosquitoes at any time of the day, but you’ll want to be especially well prepared in the evenings.
Where
As well as understanding the seasonal and day-to-day patterns of mosquito activity (especially in temperate climates), it’s also crucial to have an idea of where you’re most likely to come across mosquitoes.
Mosquitoes are commonly found close to standing water, which is abundant in boggy areas, swamps, marshes and wetlands. This is why the interior tracts of Norway tend to be more afflicted by mosquitoes than the Western coastal regions.
Malaria was originally believed to be caused by the vapours emitted by swamps before people realized it was the mosquitoes giving them the disease. They at least knew to avoid swamps.
On a more local level, mosquitoes can also be highly active near small lakes, ponds, ditches, puddles, drains or anywhere else where conditions are suitable for breeding.
Mosquitoes also love to hide in forests and jungles where they enjoy the shelter from the wind and the protection from the harsh sun. Entering their dominion is always asking for trouble.
During the summer months in Maine, I remember getting chased by swarms of extremely aggressive mosquitoes every time I would step into the woods.
They would bite through clothes and would even try to burrow through the shoelace holes in my shoes to gain access to my feet where they could bite through my socks.
One day I suffered more than 100 bites on my back through my long-sleeved shirt when I was lounging in the woods. But outside of the woods the mosquitoes were nowhere to be seen.

You know the scenario. During a long, sweaty hike you decide to stop for a breather at a convenient rest spot next to the trail.
You plonk yourself down on a fallen log and wipe the sweat from your brow. At first, nothing seems to be amiss, with no sign of any airborne pests.
Then suddenly, a solitary, droning mosquito appears out of the blue, followed by another, and then another. Within the span of just a few minutes there’s an entire swarm of them surrounding and harrying you.
The burning question is: how did these mosquitoes find you?
Well, one of the ways that mosquitoes detect your presence is by the carbon dioxide gas in your breath when you exhale. Your skin pores are also continuously emitting carbon dioxide, albeit a smaller amount.
Mosquitoes can detect this long before they can see or smell you, even from more than 150 feet way if the CO2 concentration is high enough.
Mosquitoes can also smell many of the compounds in human perspiration thanks to a number of olfactory receptors found on their antennae.
Human sweat is an intoxicating cocktail of compounds like acetone, sulcatone, lactic acid and carboxylic acids that mosquitoes pick up on and find irresistible. They use these scents to home in on you after initially detecting the carbon dioxide from further away.
Once mosquitoes get to within 5 to 15 metres they can use visual cues to lock onto the target and once they’re within inches of their meal, they can sense the victim’s body heat.
Sadly, there’s nothing you can really do to avoid producing these mosquito attractants, because you have to breathe out carbon dioxide, perspire and produce heat to survive.
You can however try to consciously sit still and slow your heart rate and breathing, so that you produce less carbon dioxide, perspiration and maintain a lower body temperature. The mosquitoes will still sniff you out eventually, but it will take them longer.
Experienced meditators who can significantly slow their breathing and heart rate to the point where they appear to be almost dead can still be bedevilled by a mosquito that shows up to bite a patch of exposed skin or simply to buzz around the ears and cause disturbance.
Advanced meditation practitioners learn not to become irritated or angry at the mosquito in this type of situation and to brush it off in a dispassionate manner.

Mosquitoes tend to most frequently bite the back of the hands, wrists, top of the feet, rear of the neck, ankles and the lower legs (if they’re not too hairy).
The back is also a common target for those lounging in hammocks, where a person can easily get bitten through the fabric of their t-shirt.
Mosquitoes also like to go for the skin around your hips and waist whenever your shirt inadvertently lifts up and exposes that region.
One factor that makes a part of the body relatively attractive to mosquitoes is if it tends to be relatively hairless, as thick hairs can act as a barrier that prevents mosquitoes from reaching the skin. Wrists, ankles, and necks are normally less hairy than many other parts of the body.
In the case of your hands, wrists and neck, they’re often the only parts of the body (apart from the face) that remain exposed when everything else is covered up by clothing, which also helps to explain why they get bitten more.
For the back of neck specifically, it’s a place where you can’t see what’s going on or be sure if a mosquito has landed on you, so mosquitoes have learned to take advantage of that vulnerability.
More than anywhere else on your body, mosquitoes probably most love to bite your feet.
One likely reason is that your feet are the part of your body that’s furthest away from your (potentially lethal) swatting hand.
It’s also easy to overlook what’s going on at your feet, since they’re far away and people don’t normally look down at their feet when sitting or standing still. Mosquitoes thrive on our lack of awareness.
The feet (and wrists) also have a thin layer of skin, which makes it easier for mosquitoes to tap into the network of capillaries just below it.
Ever wondered how exactly mosquitoes accomplish the task of drawing blood from your veins and how they often manage to do so without you even noticing?
The secret lies in the female mosquito’s very specialized and sophisticated mouthparts. The distinctive, elongated proboscis that mosquitoes use to siphon your blood is a lot more intricate than a simple straw.
The proboscis actually consists of an outer sheath known as the labium, which encloses and protects an array of six probing needles, which all play an important role in the feeding operation.
You can actually see this sheath retract and bend away from the six-needle core when the mosquito begins piercing your skin.
The labium has two sensory probes or labella at its tip; these aid the mosquito in locating a suitable spot to begin probing for a blood vessel. The labella can be thought of as the lips of the mosquito and they remain on the surface of the skin while the six needles pierce it.
The six needles that penetrate your skin are known as stylets (probes)and collectively they are known as the fascicle. The fascicle is comprised of a pair of mandibles, a pair of maxillae, the hypopharynx and the labrum.
The maxillae have serrations at their tips that are used by the mosquito to saw through your skin tissues.
While the maxillae are at work, the mandibles are being used to hold the skin tissues apart, kind of like how you’d hold your steak steady with your fork while cutting it with your knife.
Meanwhile, the hypopharynx, which has a minute salivary duct along the length of its underside, is channeling saliva (containing a mixture of proteins) into the tissues.
The saliva proteins act as a mild anesthetic, suppress the victim’s immune response, counteract blood-clotting and dilate the animal’s blood vessels to ensure an uninterrupted flow of blood.
The proteins in a mosquito's saliva are also responsible for that itchy bump you often get after a mosquito bite. Diseases are also transmitted through the saliva.
The anesthetic in the mosquito’s saliva explains why you often don’t realize you’ve been bitten until the itchy bumps appear on your skin.
Once the mosquito’s proboscis has penetrated your skin, it uses the gutter-shaped labrum (which has blood-sniffing receptors) to probe around underneath the skin surface for a suitable blood vessel.
Once a suitable, active blood vessel is located and subsequently pierced, the hypopharynx and the horseshoe-shaped labrum come together to form a sealed tube.
While the hypopharynx continues to inject saliva, the victim's blood is siphoned up through the labrum to be collected in the mosquito’s abdomen.
As the female’s abdomen fills with blood, she is able to separate the water content from the red blood cells and squeeze it out from the tip of her abdomen, thereby concentrating the nutrients and freeing up space for her to ingest more blood.
Her habit is to try to extract as much blood as possible in each feeding session due to the difficulty and the potential danger involved in finding another host.
Check out the video that we've embedded above also for a visual understanding of the feeding process.

The characteristic itchy, swollen, red bumps or wheals that appear after receiving mosquito bites are actually caused by your body’s own mild allergic reaction to the enzymes and proteins in the mosquito’s saliva, which is injected into you while the mosquito is sipping your blood.
In response to these foreign substances that have been introduced into your body by the mosquito, your immune system sends IgE (immunoglobulin E) antibodies to the site of the bite.
These antibodies bind with mast cells and trigger the release of a type of protein called histamine from the cells.
The histamines cause the blood vessels at the site of the bite to dilate, thereby increasing the blood flow and bringing in more white blood cells to fight the perceived foreign invader.
However, the dilated blood vessels can also leak some fluid, which causes the swelling (red bumps) associated with mosquito bites. The itching is also caused by the histamine when it tickles your skin’s itch receptors.
People react to mosquito bites to different degrees and most people may become more tolerant with repeated exposure, which is why adults usually react less than kids.
However, very young children who have never been bitten before may not experience any itching or swelling since the body has not yet produced antibodies for mosquito bites.
A few people can actually become more sensitive to the mosquito’s saliva with repeated exposure and in certain cases a bite can cause a person to go into anaphylactic shock.
This is a severe allergic reaction to mosquito bites that results in major swelling and causes airways to narrow, making it difficult or impossible to breathe. Thankfully, this reaction is very rare and chances are that you don’t need to worry about it.
In most cases, you just need some relief from the swelling and itching.
Some of the popular treatment options for relieving the itching and inflammation caused by mosquito bites include:
Calamine & Caladryl
.jpg)
Calamine is an over-the-counter (OTC) medicine that comes as a bubblegum-coloured cream, lotion or ointment and that’s used to relieve mild itching (pruritis), although it doesn’t address the inflammation caused by mosquito bites. It’s made from a pinkish powdery mixture of (mostly) zinc oxide and ferric oxide that goes by the same name.
Caladryl lotion is another very similar over-the-counter antipruritic medicine. The “dryl” in the name comes Benadryl, which was removed from the formula in the 90’s when it was causing some kids to experience hallucinations when liberally applied.
Caladryl now contains calamine and a local anaesthetic called pramoxine (also pramocaine or pramoxine HCL) to dull the nerves at the site of the bite and trick your brain into thinking there’s no itch.
Hydrocortisone
This over-the-counter medicine is a corticosteroid (not an antihistamine) that usually comes in ointment, cream or lotion form with 1% hydrocortisone.
You would normally only use this medicine for more severe allergic reactions to mosquito bites. If the itching and swelling is milder, one of the other remedies mentioned here would be more appropriate.
Hydrocortisone works by blocking the release of histamines from mast cells, thus reducing the itching and inflammation associated with a wide variety of skin conditions, including mosquito bites.
Oral antihistamines
Another option to reduce inflammation is to take an oral antihistamine like Benadryl. These give relief throughout your entire body by reducing your body’s response to the histamines.
Oral antihistamines are especially useful for when you’re having trouble sleeping because the older first generation histamines can cause drowsiness as a side effect.
However, the newer second generation histamines like cetirizine (Zyrtec) and Ioratadine (Claritin) can be taken during the day and won’t have a sedative effect.
Ice packs

An ice pack will have a vasoconstricting effect in the bite area to contract and will also numb the skin, thus helping to reduce the swelling and pain from the bite.
Green tea bags

A green tea bag dampened with cold water and placed over the inflamed area can provide relief great relief, not only because of the cooling effect of the tea bag but also because the tannins and caffeine in tea help to constrict the blood vessels and reduce swelling.
Green tea works particularly well because it contains much higher levels of an anti-inflammatory compound called EGCG (epigallocatechin gallate) than black tea.
The short answer to this is "no".
Most people can probably recall a scenario in their lives where they got completely annihilated by mosquitoes while their companion didn’t suffer so much as a single bite, or vice versa.
This happens because some people are just more attractive to mosquitoes than others, although the exact underlying reasons for this remain something of a mystery.
Some scientists believe that genetics account for about 80% of the factors that make you attractive to mosquitoes, but there are other important non-genetic factors at play as well.
In a study conducted by Japanese researchers it was discovered that test subjects with Blood Type O were significantly more attractive to the Asian tiger mosquito (Aedes albopictus) than those with Blood Type A, while those with Blood Type B fell somewhere in between in terms of attractiveness.
Researchers have also found that mosquitoes find pregnant women more attractive than non-pregnant women.
This might be because pregnant women exhale a greater volume of air and have slightly hotter abdomens (causing more volatiles to be released from the skin) than non-pregnant women, making it easier for mosquitoes to detect their presence.
Heavy breathers are also at increased risk of being made a meal of, since they exhale more mosquito-attracting CO2 with each breath.
The skin microbiota are believed to be a major (largely non-genetic) factor in influencing a mosquito’s choice of target.
Skin microbiota are the healthy bacteria, fungi and other microbes that live on our skin and inside our pores and hair follicles.
Everyone has a different skin microbiota composition that is largely determined by our environment (the things we touch, eat and drink) and to a lesser extent, our genetics.
It’s understood that mosquitoes find some compositions more attractive than others, although exactly which ones they prefer and why is still not clearly understood.
Body odour, which is unique to every individual and is partly influenced by our skin microbiota, is another factor that must surely play a role in a mosquito's preferences.
Mosquitoes can carry a number of dangerous viruses and parasites, which they often contract while feeding on infected birds, nonhuman primates, domestic animals and previously infected humans.
Under some circumstances, infected mosquitoes are unable to transmit the diseases that they carry to humans but given the right conditions, transmission can occur, often resulting in major outbreaks.
In many tropical regions that have just two distinct seasons, dry and rainy, outbreaks of mosquito-borne illnesses are associated with the rainy or monsoon season, so travellers should bear this in mind when planning their trips.
All in all, over half the world’s population in more than 125 countries is at risk from diseases spread by mosquitoes. Almost 700 million cases of mosquito-borne illness are believed to occur each year, resulting in over 1 million deaths.
There are dozens of diseases that mosquitoes transmit to humans but many of these are rare enough that you needn't worry about them.
What follows is a list of the most dangerous and commonly reported mosquito-borne illnesses that you ought to be clued in about as a traveller.
Malaria
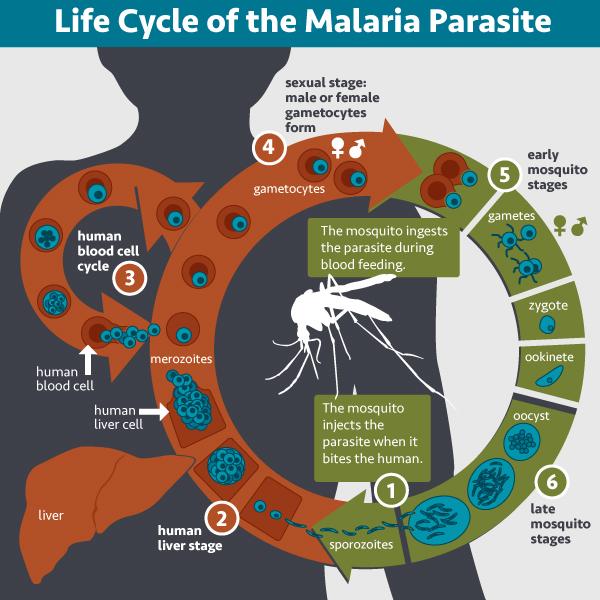
Malaria is the mosquito-borne illness that the majority of people are probably most familiar with.
The word "malaria" has its roots in the Latin malus aria, meaning “bad air”, as it was believed by the Romans that the disease was caused by breathing in the noxious vapours emitted by swamps.
The illness is highly prevalent in sub-Saharan Africa, where it presently claims over 400,000 lives annually, with over half the victims being children under 5 years of age.
Africa currently accounts for about 90% of the total global malaria deaths, a trend that is largely due to the lack of access to treatment in this part of the world.
Historically, malaria was prevalent in Europe, North America and in other non-tropical regions, but over time it has been virtually eradicated from everywhere except the tropics.
Much progress has been made against the disease in recent years, with the total number of deaths from malaria having almost halved between 2000 and 2015.
The 40 or so mosquito species that commonly transmit the Plasmodium parasites that cause human malaria are all from the Anopheles genus, which has about 460 species in total.
Anophelines seem to be particularly susceptible to infection by malaria parasites and also have a preference for feeding on humans or on other animals like cattle and birds, making them vectors for the disease.
These mosquitoes also live long enough in their adult stage for the malaria parasite to complete its reproductive cycle.
There are five recognized Plasmodium parasites that cause malaria in humans, namely P. falciparum, P. vivax, P. ovale, P. malariae and P. knowlesi.
P. falciparum causes the most severe form of malaria, while P. vivax and P. ovale are known for their ability to hibernate in the liver, which can give rise to relapses several weeks, months or even years after the patient is apparently cured.
P. malariae causes a more benign form of the illness and is known for causing fevers that recur at 72-hour intervals (instead of the usual 48-hour intervals), while P. knowlesi is a malaria strain that's restricted to Southeast Asia and that can cause a severe form of the illness.
Once the malaria parasite enters the human body in the saliva of an infected mosquito, it hitches a ride to the liver, where it infects cells and begins to multiply, creating thousands of new parasites.
These parasites are then released back into the bloodstream where they invade red blood cells and produce as many as 36 daughter parasites while protected from the human immune defenses inside the cells.
At maturity, the red blood cell bursts, releasing large numbers of malaria parasites back into the bloodstream where they go on to infect other red blood cells, thus continuing the cycle of destruction.
From the initial time of infection, it normally takes at least 12 days for symptoms to appear, but can take 40 days or longer, depending on a number of factors.
The symptoms of malaria begin during the stage where the parasite begins infecting red blood cells and they include high fever, chills, profuse sweating, nausea, vomiting, diarrhea, headache and in some cases the illness can progress to coma and death.
However, if diagnosed early and treated correctly with the appropriate antimalarial drugs, the prognosis for malaria is excellent.
It normally takes about 2 weeks of treatment to be fully cured of malaria, although in some cases, as we mentioned earlier, relapses can occur several weeks, months or even years later, even when the patient was apparently cured.
One of the rare complications that can occur with the illness is cerebral malaria, where red-blood cells that are infected with malaria parasites clog the blood vessels supplying the brain, potentially leading to brain damage, swelling, coma, seizures and death.
If the illness progresses this far the patient only has an 80% chance of survival, even when good treatment is available.
Dengue fever

Dengue fever is the one mosquito-borne illness that I keep hearing about travellers falling prey to time and time again. This is unsurprising consider that Dengue is the most common viral disease transmitted by arthropods.
Dengue is an illness associated with the tropics and subtropics in many parts of the world including Latin America, the Caribbean, Africa, India and Southeast Asia.
Unlike malaria, which is on the decline, dengue is a growing problem across the globe and the incidence has increased more than 30-fold in the last 50 years.
Back in 1970 only 9 countries were facing serious Dengue outbreaks and now the illness is continually present in over 100 countries.
The disease now threatens 3 billion people or approximately 40% of the world population in over 100 countries and infects as many as 400 million people worldwide each year.
Of those 400 million who get infected, about a quarter fall ill and 22,000 succumb to the disease. As with malaria, young children are particularly vulnerable.
While Dengue doesn’t kill anywhere near as many people as malaria, it nonetheless causes a lot of economic loss and human suffering.
Dengue is caused by four related flaviviruses (DENV-1, DENV-2, DENV-3 & DENV-4) and the primary transmitters of these viruses to humans are the female Aedes Aegypti and Aedes albopictus mosquitoes.
These two dengue-carrying species bite during the day and night and can also spread other viruses like Zika and Chikungunya.
Symptoms of the illness usually appear within 3-7 days after transmission and normally consist of high fever, chills, headaches, acute aching pain in the bones and muscles (leading to the moniker “break-bone fever”), pain behind the eyes and red skin rashes.
The fever typically runs its course within 7 days, although one of the complications that can develop after the fever subsides is dengue hemorrhagic fever, also known as severe dengue.
Severe dengue is characterized by leakage of plasma from blood vessels, gastrointestinal bleeding, blood appearing in stools and urine, frequent vomiting, stomach pain, breathing difficulties and febrile seizures.
About 90% of the patients that develop severe dengue are below the age of 15 years and overall fewer than 5% of Dengue victims will develop the complication. For those that do develop severe dengue, the fatality rate is as high as 2.5%, though it falls below 1% if proper treatment is available.
As it’s a viral illness, antibiotics are ineffective against Dengue and treatment involves getting plenty of rest, fluids and taking antipyretics and anodynes like paracetamol (acetaminophen) to control the fever and to alleviate the aching pain.
Unfortunately, contracting Dengue and recovering from it doesn’t confer lifetime immunity since there are still three other strains of the virus that could potentially strike next time.
Indeed, prior infection with one of the Dengue virus strains may leave you more susceptible to developing severe Dengue the next time round.
West Nile Virus (WNV)
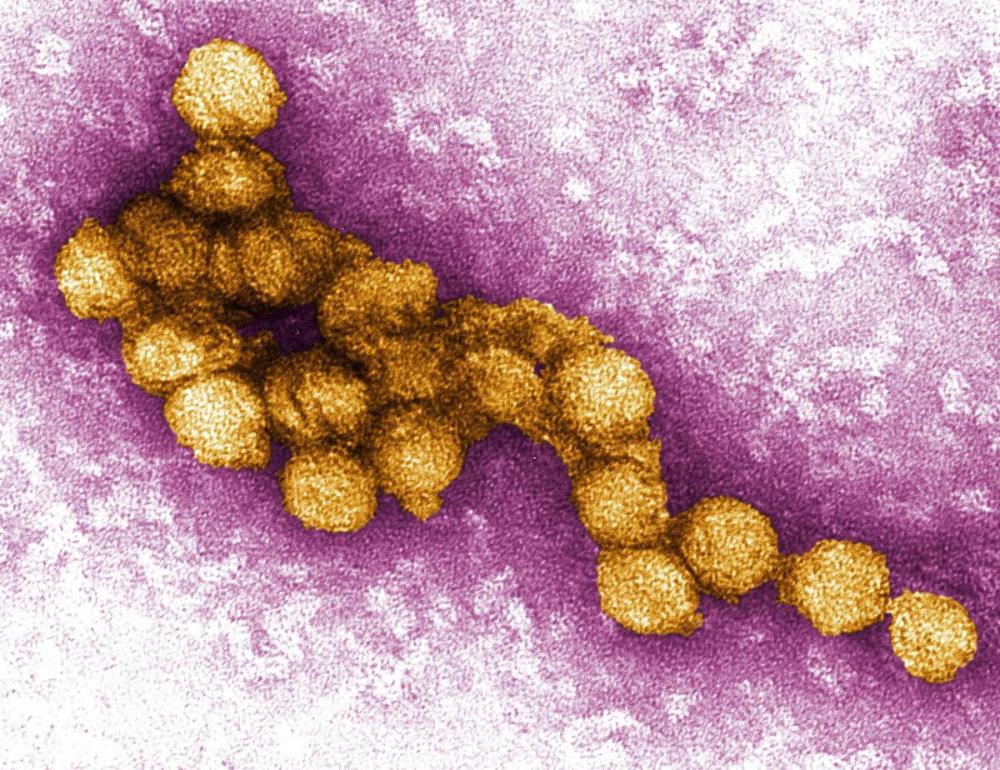
West Nile Virus is a mosquito-borne illness that was first isolated in 1937 from a woman in east Africa, in a part of Uganda known as the West Nile district, hence the name.
The mosquito-borne virus behind this illness belongs to the Japanese encephalitis complex of the flavivirus genus (of the family flaviridae), which has 68 known viruses, 30 of which are known to cause disease in humans.
WNV is predominantly transmitted by mosquitoes of the genus Culex, although the virus has been isolated from 43 other mosquito species. In the US the three main vector species are Culex pipiens (common house mosquito), Culex quinquefasciatus and Culex tarsalis.
West Nile Virus is the most widely distributed arbovirus (arthropod-transmitted virus) and occurs in North America, Africa, Europe, the Middle East, South Asia (where it is endemic) and Western Asia. The disease is virtually absent from Latin America.
The first major outbreak of WNV in the US occurred in New York city in 1999 and the disease has been spreading throughout the American continent ever since.
Large outbreaks have also occurred in many countries on the other side of the Atlantic, including Israel, Russia, Romania and Greece. These outbreaks normally occur along important bird migration routes.
Mosquitoes first contract the virus while feeding on the blood of infected birds, which may be dead or alive. The virus is then transmitted to humans through the mosquito’s saliva.
Symptoms of infection typically begin to appear within 3-14 days, though in about 80% of cases of infection with WNV, humans are asymptomatic, but in the other 20% of cases West Nile Fever will develop.
The flu-like symptoms include a fever, headaches, vomiting, nausea, muscle pain (myalgia), joint pain (arthralgia), skin rashes and (occasionally) swollen lymph glands.
Symptoms normally subside within 3-6 days, although complications develop in about 1 in 150 cases, where the virus reaches the brain and begins to disrupt the central nervous system and cause encephalitis (inflammation of the brain tissues).
Signs that the patient has developed a more acute form of the illness include more alarming symptoms like high fever, stiff neck, convulsions, paralysis, disorientation and coma.
If the victim’s condition continues to deteriorate it could lead to death. Even those who survive this critical stage of the illness may end up with brain damage.
Although West Nile Virus isn’t anywhere near as deadly as malaria or dengue, the immunocompromised and the elderly (50+ years old) are particularly vulnerable to developing complications.
As with Dengue fever, there is no specific medication available to treat West Nile Virus, so patients should receive plenty of rest, fluids and medication to control fever and reduce pain. If symptoms worsen the patient should be hospitalized immediately.
Yellow fever

Yellow fever is yet another mosquito-borne viral illness caused by a member of the flavivirus genus.
The disease is believed to have originated from somewhere in Africa, but is now commonly found throughout much of Africa and Latin America.
The virus that causes yellow fever is transmitted by Haemagogus and Aedes mosquitoes and in particular Aedes aegypti, the species that also transmits Dengue, Chikungunya and other viral illnesses to humans.
The yellow fever virus normally circulates between monkeys and mosquitoes in the wild (known as sylvatic or jungle yellow fever) and between mosquitoes and humans when outbreaks in urban areas occur.
If it is true that the virus is not endemic to the Americas but was brought there from Africa, it’s likely that the African slave trade in the mid-1600s played a major role, where thousands of negro slaves were being shipped from West Africa to islands in the Caribbean, where their labour was required for the sugarcane plantations that were beginning to thrive here under the English colonists.
Aedes aegypti mosquitoes carrying the yellow fever virus would have hitched a ride across the ocean on these unsanitary slave ships and their arrival coincided with the New World’s very first yellow fever outbreak in Barbados in 1647.
One plausible theory holds that the deforestation and alteration of the island’s ecology as a result of the island’s sugarcane industry created conditions that were highly favourable for the proliferation of the yellow fever mosquito.
Slaves were often re-exported from Barbados to other colonies in the West Indies or North America, so the yellow fever virus was easily able to spread throughout the Americas once it had gained an initial foothold here in Barbados.
According to WHO estimates, yellow fever infects about 200,000 people annually and kills about 30,000, although the actual reported numbers are far lower. Almost 90% of cases are reported from African nations.
In the majority of cases, the virus only causes a mild illness that typically includes typical flu-like symptoms like headache, fever, nausea, vomiting, muscle aches and joint aches. These typically come on within 3-6 days of becoming infected.
In about 15% of cases however, the illness can progress to a critical phase that is characterized by recurring fever, jaundice (yellowing of the skin and eyes that is caused by liver damage) and bleeding from the eyes, nose, mouth and stomach.
Patients that reach this severe stage of yellow fever may puke up blood, which is why the Spanish named the disease vomito negro (black vomit).
In malignant yellow fever, the most severe form, there can be intractable hiccups, seizures, coma and organ failure.
In the more acute cases there’s only a 20-50% chance of survival, while the overall fatality rate for the illness is 5%, which is relatively high.
As with other viral infections, there is no specific drug that targets yellow fever and all you can really do is rest, ensure you stay well-hydrated, take drugs like paracetamol for pain relief and ensure you’re getting the best possible treatment. In most cases of yellow fever the symptoms will begin to ameliorate after 3-4 days.
Note: Travellers arriving from regions prone to yellow fever outbreaks may have to produce proof a yellow fever vaccination certificate in order to obtain entry to certain countries. Some countries ask for this certificate from all travellers over a certain age, regardless of what country the traveller is arriving from.
Zika virus
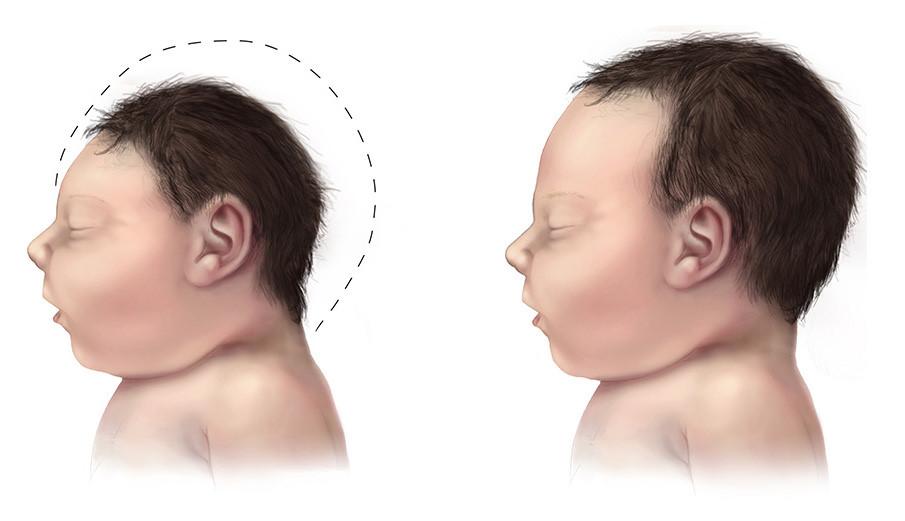
Zika is another one of the flaviviruses, the same group that cause Dengue, yellow fever and chikungunya, and it is spread by the same Aedes mosquitoes, especially Aedes aegypti and possibly A. albopictus as well.
The disease was first isolated in 1947 from a captive rhesus monkey in Uganda and the first human cases were detected in Uganda and Tanzania in 1952.
Although sporadic cases of the disease were reported in South Asia and Southeast Asia over the following decades, it wasn’t until 2007 that the first major outbreak of Zika occurred on the western pacific island complex of Yap (part of the Caroline island group and one of four member states in the Federated States of Micronesia).
More outbreaks of the disease occurred in 2013 and 2014 in four other Pacific islands, namely Easter Island, French Polynesia, New Caledonia and the Cook Islands.
The was huge panic over the 2016 Zika virus epidemic, where the illness spread like wildfire through Latin America and soon reached the United States where 200 people fell ill in Florida and Texas.
But then the virus suddenly went off the radar again, although health experts warn that the next major outbreak is not a matter of if, but when.
Zika virus circulates between mosquitoes and humans and is largely an illness associated with overcrowded urban slums like the Brazilian favelas. The virus can also be transmitted from person to person by sexual contact, though probably not by kissing.
Zika virus is perhaps best known for its tendency to cause the babies of infected women to be born with abnormally small heads and incomplete brain development, a condition known as microcephaly.
It can also cause Guillain-Barre syndrome, an autoimmune reaction that attacks peripheral nerves and can result in severe paralysis of the limbs, and is fatal in about 1% of cases.
Another possible complication of the illness is encephalomyelitis, an inflammation of the fatty myelin layer that protects the nerve cells in the brain and spinal cord.
In about 80% of Zika cases in adults however, the virus causes no symptoms or only mild symptoms like fever, headaches, skin rashes, muscle pain, joint pain and sometimes, conjunctivitis (redness and itchiness of the eyes).
Symptoms of the illness usually appear within 3-14 days and typically last no longer than a week. Treatment is the same as for other viral infections, with patients requiring plenty of rest, fluids and symptom-relief provided by Tylenol and similar medications.
Chikungunya

Chikungunya first came to the world’s attention in 1952 following an outbreak of the disease on the Makonde plateau, located in southeastern Tanzania near the border with northern Mozambique.
“Chikungunya” is a Kimakonde (the language of the Makonde people) word meaning “to become contorted”, referring to the stooped posture displayed by victims of the illness suffering from joint pain (arthralgia).
The virus that causes Chikungunya fever belongs to the alphavirus genus of the family Togaviridae and it is transmitted to humans by Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus.
The disease is endemic in East Africa and since its initial discovery there have been numerous outbreaks occurring at irregular intervals in Africa, Europe, India and islands in the Indian and Pacific oceans.
There have been 1.7 million suspected cases of Chikungunya in the U.S, the Caribbean and Latin America since the year 2013, when the very first case of the illness in the Americas was reported.
In total to date, the disease has been reported in over 60 countries across Africa, Asia, Europe and the Americas.
The virus circulates between humans and infected nonhuman primates in its native range but, as with other mosquito borne viruses, can cause epidemics when infected humans enter urban areas with large numbers of naïve hosts and Aedes mosquito populations.
Symptoms of the illness include sudden high fever, headache, nausea, joint pain (often with swelling), muscle pain and rashes. Due to the similarity of the symptoms, chikungunya is often misdiagnosed as Dengue. Onset typically occurs within 3-7 days of infection and the body takes about 5-7 days to clear the virus from the system.
Treatment of the illness is similar to that for other viral illnesses, being aimed at relieving symptoms and ensuring patients receive adequate rest, fluids and pain-relief medication like Ibuprofen or paracetamol.
Most people recover fully in three to ten days, although in a high percentage of cases chronic joint pain can plague victims for months or even years after recovery.
Fortunately, the fatality rate for Chikungunya fever is very low (less than 1 in 1,000) and it is usually only elderly people that succumb to the illness.

There are vaccines currently available for a select few mosquito-borne illnesses but for most experimental vaccines are still undergoing clinical trials.
Before deciding to get vaccinated against a mosquito-borne illness you should research how safe, effective and costly the vaccine for it is, and whether you are travelling to a region where you could be at risk from that particular disease.
Your local GP will also weigh in with his opinion, but beware of the potential for financial incentives to skew recommendations. Some doctors can be inordinately eager to prescribe vaccines for diseases that patients will be at very low risk of contracting.
Malaria vaccine
Although there are a few candidates that have shown promise, there is currently no licensed malaria vaccine available on the market.
The malaria parasites are extremely complex and their remarkable ability to evade the human immune defenses may explain why there is still no effective vaccine for the disease after decades of research.
Some travellers do take antimalarials if travelling in high or moderate risk areas for the illness. See the next question for more info on that.
Dengue fever vaccine
There is one licensed vaccine for Dengue called CYD-TDV, which is sold under the brand name Dengvaxia.
The vaccine is delivered in three shots over the course of a year and is now commercially available in 19 countries in addition to dengue-endemic parts of Europe such as the Caribbean islands of Guadeloupe and Martinique.
In 2019 it was approved by the FDA for use in the US, but only for children aged 9-16 living in Puerto Rico and a few other offshore territories where Dengue is endemic (circulating constantly). Furthermore, children can only received the vaccine if they have previously had at least one confirmed case of Dengue.
The French drugmaker Sanofi Pasteur that manufactures the vaccine cautions that the vaccine is only recommended for those that have previously been infected with Dengue.
Those who are naïve to the Dengue virus (i.e were never were infected previously) may be at a slightly increased risk of developing severe Dengue and a dangerous complication known as plasma leakage syndrome if they get infected after being vaccinated.
This happens because of a phenomenon is known as antibody dependent enhancement (ADE), where antibodies created by exposure to one strain of the virus act as “double agents” in the case of a second infection by a different strain of the virus.
The antibodies created by the first strain actually assist the second strain to bypass the immune system and the Dengue vaccine effectively acts as that first strain of the virus.
Back in 2017 there was a big controversy over the vaccine in the Philippines, which was the first Asian country to approve the commercial sale of Dengvaxia.
Between April 2016 and November 2017, the vaccine was administered to over 700,000 Philippine schoolchildren in a Government-sponsored campaign that began in Manila.
The controversy arose over the fact that the vaccine was rolled out with undue haste and was given indiscriminately; at least 100,000 kids that were seronegative (had not previously contracted Dengue) received the shot.
The manufacturer Sanofi only acknowledged the potential risk to kids who had not contracted Dengue previously in late November 2019 after hundreds of thousands of kids had already been vaccinated and about 600 had died of internal bleeding, especially in the brain and lungs.
The announcement from Sanofi triggered mass panic and hysteria among the public and many parents began to suspect that the deaths of their children were caused by the vaccine. The sale of the vaccine in the Philippines was suspended a few days later, over a year after the campaign had begun.
In the following months, the Government launched investigations and performed autopsies on children who had died after receiving the shot.
14 Philippines health officials and 6 Sanofi employees are now being indicted for reckless imprudence resulting in homicide relating to the deaths of 10 children.
As of February 2019 the Dengvaxia vaccine has been permanently banned from the Philippines by the authorities.
One of the side effects of the controversy was the plummeting of public confidence in the country’s immunization program (including those that people previously trusted), which some people are linking to a surge in measles cases in the country.
West Nile virus vaccine
Although there are several vaccines approved for the disease in horses, there is currently no licensed WNV vaccine that protects people from the illness.
The NIAID (National Institute of Allergy and Infectious Diseases) website provides a list of vaccines that are currently under development for West Nile virus.
Zika virus vaccine
There is no commercially available vaccine for Zika Virus, although multiple vaccine candidates are currently undergoing clinical trials.
Yellow Fever vaccine
There is a licensed vaccine for yellow fever and as we mentioned earlier, you may require a vaccination certificate proving you have received this vaccine in order to be admitted to certain countries, especially if you’re arriving from a yellow fever hotbed.
The WHO maintains a list of the proof of yellow fever requirements of every country in the world.
The yellow fever maps on the CDC website will tell you if you’re travelling to a high-risk zone or arriving from one.
Most authorities recommend the vaccine for anyone over the age of 9 months travelling to parts of Africa and South America where the disease is endemic.
The yellow fever vaccine in use today is the results of much trial and error and many failed attempts.
The vaccine is called 17D and has been around since 1937 when it was first discovered at the Rockefeller Institute in NYC by a South African virologist named Max Theiler.
In 1951 Theiler won the Nobel Prize in Physiology or Medicine for his work on the vaccine, becoming the first African-born Nobel laureate.
The yellow fever vaccine typically costs around $50 to $100 per dose in the US, with prices being much lower in developing countries.
Vaccination involves getting injected with a live, attenuated form of the yellow fever virus and a single dose is believed to confer lifetime immunity for most people.
However, it takes 10-30 days for people to become fully protected after receiving the shot, so travellers are advised to get the vaccine at least 10 days before travelling.
Chikungunya vaccine
There is presently no vaccine available to prevent Chikungunya.
One live attenuated vaccine candidate named VLA1553 is currently being developed by French Biotech company Valneva and is showing promise so far.
Themis, an Austrian Biotech company, has also developed its own experimental Chikungunya vaccine, which has had a positive phase II trial and has plans to begin phase III in 2020.
Because of the potentially adverse side effects they can cause, not to mention the financial cost, antimalarials are usually only prescribed for travellers heading off to regions that are at high risk for malaria.
The disease mostly affects the tropics and subtropics at elevations below 1,500 metres but the risk varies considerably depending on the exact part of the world you're travelling to.
For example, the risk of contracting malaria is high across much of Sub-Saharan Africa and in Papua New Guinea, moderate in India, Myanmar and Indonesia, and low in most South American countries.
The following distribution map shows the incidence of malaria per 1,000 people at risk and gives an idea about where you need to be most careful.

Another thing to bear in mind is the cost involved with getting prescribed anti-malarial medication.
There is the cost of the medication itself, which varies according to what drug you choose, and also the cost of making an appointment with your doctor if you choose to go the offline route.
Some people prefer to buy antimalarial drugs online to avoid the cost of a doctor's appointment, though in that case you'll want to have done enough of your own research to be confident you're buying the right medication.
Antimalarial drugs can be much cheaper when purchased abroad, but in some countries there is a risk that they will be of poor quality, contaminated, out of date or even completely counterfeit and therefore totally ineffective. It's considered more prudent to buy all the tablets that you need before you go abroad.
There are also the potential side neuropsychological effects of some of these drugs to consider, which can include insomnia, anxiety, depression, dizziness, confusion, hallucinations and psychosis, in addition to the more common physical side effects like nausea, vomiting, diarrhoea, headache, tinnitus and abdominal pain.
Most antimalarial prophylactics also have a few contraindications with some for example, being unsuitable for pregnant or breastfeeding women or for children under a certain age. People with genetic conditions such as G6PD also have to be careful not to take the wrong medications.
Moreover, there’s no guarantee of protection with antimalarial prophylactics, even if you diligently take the correct dosage at the correct intervals for the entirety of your trip.
This is why antimalarial medication should always be combined with other safety measures like covering up during mosquito feeding times and using topical and spatial repellents.
There are a number of reasons why antimalarial drugs cannot ever be counted on to protect you 100% of the time.
The first issue is that mosquitoes in certain pockets have developed resistance to certain drugs. Chloroquine is one anti-malarial drug for which resistance is now widespread and Mefloquine is no longer effective in many parts of Southeast Asia.
P. falciparum malaria parasites in the Greater Mekong sub-region (Laos, Cambodia, Vietnam, Southern China, Myanmar & Thailand) are especially adaptable and have shown greater drug resistance here than P. falciparum parasites in other parts of the world.
The other issue with antimalarials is that standard dosages can be less effective on large or overweight people and differences in people’s ability to metabolize the drugs can also give rise to variations in efficacy.
Anti-malarial medication is usually started a few days before travel (so that the drug has time to reach sufficient levels in your blood), is taken at regular intervals (usually daily or weekly) for the duration of the trip and is then continued for as long as four weeks after leaving the affected region, since parasites can still emerge from the liver during this period.
The most commonly prescribed anti-malarial drugs today are Atavaquone/Proguanil (Malarone), Doxycycline and Mefloquine (Lariam). Chloroquine, Primaquine and Tafenoquine may also be recommended in certain cases.
Depending on where you are in the world, some of these drugs may be bought over the counter from pharmacies or online without a prescription.
We'll now briefly discuss each of these popular antimalarial drugs and outline their associated pros and cons for travellers.
Malarone (Atavaquone/Proguanil)
Malarone is the brand name of a medicine that combines two separate anti-malarial drugs, namely Atavaquone and Proguanil.
It was first patented to treat malaria in 1999 by Glaxo Wellcome, which merged with another British pharmaceutical company called SmithKline Beecham in 2000 to form the pharmaceutical giant GlaxoSmithKline.
Malarone is often prescribed for travellers visiting areas where mosquitoes have developed resistance to Chloroquine or other anti-malarial drugs.
According to goodrx.com, the average retail price in the U.S for a 1-month supply of thirty 250mg/100mg adult tablets is $187.89, making this the most expensive anti-malarial drug on our list.
The usual dosage for adults is one 250mg/100mg tablet taken daily. Low-dosage pediatric tablets are also available for children, with the exact dosage depending on the weight of the child. Once children weigh 40 kg or more they are prescribed the adult tablets.
Travellers only need to start taking the tablets 2-3 days before heading off and for just 7 days after leaving the malaria-prone region, making this drug a good choice in the case of last-minute travel plans and/or shorter trips.
Something important to be aware of however is that in many European countries Malarone is only registered for use not exceeding 28 days, although this restriction does not apply in the US and in other countries outside of Europe.
Common side effects observed with Malarone are vomiting, diarrhea, abdominal pain, headache, indigestion and dizziness.
More serious and less common side effects may include anaphylactic shock, hallucinations, Stevens-Johnson syndrome (a disorder of the skin & mucous membranes), liver damage and many others.
Malarone is not suitable for women that are pregnant or breastfeeding a small child and it’s not ideal for those who’d rather not have to take tablets on a daily basis.
Chloroquine
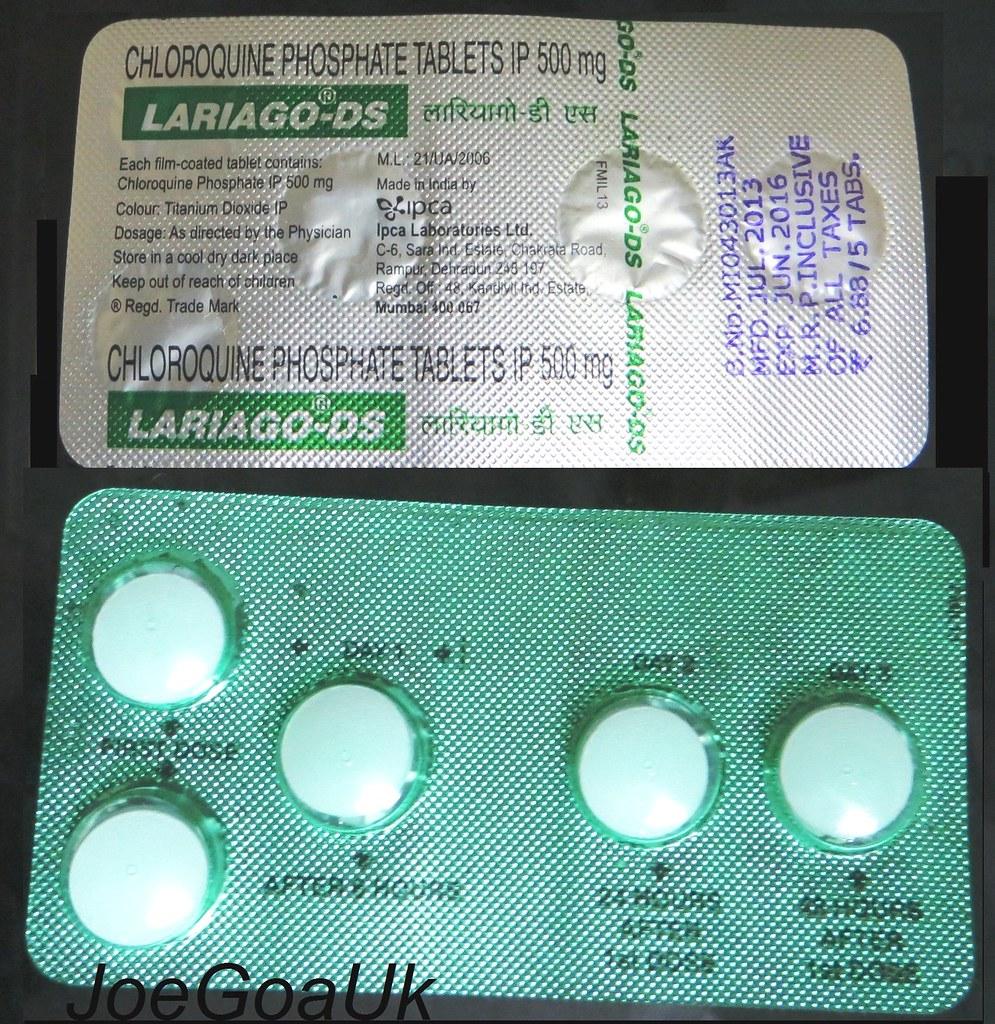
Chloroquine (also chloroquine phosphate) was first discovered in 1937 by German scientist Hans Andersag and his co-workers while they were conducting research into a substitute for quinine and it became the first widely used anti-malarial drug.
The story of chloroquine began in 1937 with a group of scientists that were working for the pharmaceutical conglomerate Bayer IG Farbenindustrie at one of its sites in Elberfeld, Germany.
The scientists were conducting research into a substitute for quinine when Hans Andersag, a German scientist among them, synthesized a compound called Resochin.
The drug he had discovered was however ignored for over decade because it was considered too toxic for human use.
It was only later during World War II when the forgotten drug was re-examined in the United States. It was renamed Chloroquine and began to be viewed as having potential as an anti-malarial drug.
According to goodrx.com, the average retail price for a 1-month adult supply of four 500 mg (300 mg base) chloroquine phosphate tablets is $56.05.
As regards dosage, those already taking hydroxychloroquine for rheumatologic ailments may not require any additional medicine, but for normal adults, the recommended dosage of Chloroquine is one 300 mg base (500 mg salt) tablet taken once a week.
The dosage for children is 5 mg base (8.3 mg salt) per kg taken orally once per week, up to a maximum of 300 mg base (500 mg salt). It should not be given to children younger than 8 years.
With the medication only having to be taken once per week, it’s a good option for for longer trips. Another plus is that Chloroquine is considered safe for women during all three stages of pregnancy.
Like other anti-malarial drugs, Chloroquine can cause a host of side effects, including loss of appetite, diarrhea, headache, nausea, abdominal cramps and blurred vision.
More serious side effects may include, muscle damage, sunlight sensitivity, blurred vision, vomiting, fever, tinnitus, hearing loss, hair loss, seizures and many others.
One major downside is that the drug needs to be started 1-2 weeks prior to the commencement of the trip, making it an unsuitable choice in the event of last-minute decisions to travel.
Chloroquine also needs to be continued for 4 weeks after a trip ends, making it a less desirable choice for short trips.
One major issue with Chloroquine is that the Plasmodium falciparum malaria parasite has developed resistance to the drug almost everywhere in the world that this type of malaria parasite is transmitted.
Another plasmodium malaria parasite, P. vivax, has also developed resistance to Chloroquine in Papua New Guinea, Southeast Asia, Ethiopia, Madagascar and possibly in other parts of the world too.
Because of the problem of widespread resistance, Chloroquine is now mainly only prescribed for travellers heading to the Middle East, Central America, Haiti and the Dominican Republic.
Doxycyline

Doxycycline is an antibiotic that was invented and developed back in the 1960s by Pfizer inc. , the multinational pharmaceutical giant that’s headquartered in New York. The drug is marketed under the brand name Vibramycin among several others.
According to goodrx.com, the average retail cost of a 1-month adult supply of 30 doxycycline hyclate 100 mg capsules is $117.15.
An equivalent supply of the other form of the drug, doxycycline monohydrate, is much cheaper however, with an average retail price of $59.14. This often works out to be the least expensive of all antimalarials and just as effective as the other form of the antibiotic.
People suffering from acne may already be taking this antibiotic drug chronically and won’t require any additional medication if travelling to high-risk areas for malaria.
Otherwise, the recommended dosage for adults is 100 mg taken daily. Children should be at least 8 years old to take doxycycline and the usual daily dosage for them is 2.2 mg per kg of the child’s body weight with a dose of 4.4 mg per kg given on the first day only. Children that weigh more than 45 kg are normally prescribed an adult dosage.
The medication should be taken on a full stomach with a full glass of liquid and dairy products should be avoided for a few hours after taking your dose.
Doxycycline may help to prevent other diseases (e.g Weil’s disease) too. It’s also another good choice for last-minute trips, as it can be started 1-2 days prior to trip commencement.
However, doxycycline is not an ideal choice for short trips, as the drug must be continued for 4 weeks after the trip finishes. The fact that it must be taken daily also makes it an unappealing option for long trips.
Some other drawbacks with this drug are that it is unsuitable for pregnant women and children under the age of 8 and can cause a range of side effects including increased risk of sunburn, diarrhea, nausea, vomiting, oesophageal inflammation and vaginal yeast infections (thrush) in women.
Mefloquine

Mefloquine is a synthetic drug whose structure is based on that of quinine, one of the world’s first antimalarial drugs that comes from the bark of the evergreen cinchona tree of South America.
The drug was first developed by the United States Army back in the 70’s to coincide with the start of the Vietnam war, though it only came into civilian usage in the 80’s.
Mefloquine is marketed under the brand name Lariam (among others) and has been used widely in Southeast Asia and South America. However, it is no longer recommended for travellers heading to Southeast Asia due to drug-resistance.
According to Goodrx.com, the average retail price in the US for a 1-month supply of four 250mg tablets is $61.50, making it the second most inexpensive antimalarial on our list after doxycycline.
The recommended dosage for adults is 250 mg taken once per week, while the usual dosage for children is 5 mg per kilo of body weight taken weekly. Children weighing more than 45 kg should take the 250 mg adult tablets.
With the weekly schedule, Mefloquine is obviously a good choice for longer trips. The drug is also considered safe for pregnant women.
The drug however is not a great choice for short trips because it must be continued for 4 weeks after the trip ends. It also must be started at least 2 weeks prior to departure, making it incompatible with last-minute travel plans.
Another big disadvantage with Mefloquine is that is considered to be one of the worst drugs in terms of side effects, especially psychological ones.
As well as the common side effects like nausea, vomiting diarrhea, headaches and dizziness, Mefloquine can also cause a range of neuropsychiatric effects in about 5% of people.
These include hallucinations, nightmares, vivid dreams, depression, suicidal thoughts, confusion, severe anxiety and panic attacks.
The risk of experiencing these effects is higher when the drug is mixed with alcohol, cannabis and other party drugs.
Also, the medication should not be used by people that suffer from epilepsy, heart conditions or that have any pre-existing psychiatric conditions.
In September 1999, a few thousand troops from the Australian Defence Force (ADF) were deployed to Bougainville Island and Timor-Leste and were given Mefloquine and another antimalarial drug Tafenoquine as part of clinical trials comparing their efficacy to doxycycline.
Many of these soldiers have recently come forward with allegations that the drug side effects were downplayed by researchers and that they were responsible for causing severe depression, suicidal thoughts, nightmares and other negative psychological effects.
Some veterans have claimed that their lives have been destroyed by the medication due to negative neuropsychological effects persisting for years after taking the drug.
For these reasons, Mefloquine is often considered a third-line drug and may only be prescribed by those unable to take safer antimalarial drugs like Malarone or doxycycline.
Also, as with Chloroquine, the malaria parasite P. falciparum has developed resistance to this and several other anti-malarial drugs, albeit for Mefloquine and its allies the resistance is far less geographically widespread than it is for Chloroquine.
Primaquine
Primaquine is an old synthetic anti-malarial drug (technically an 8-aminoquinoline) that first came into use in the 1950s, but has only recently been shown to be an effective prophylactic.
The drug’s discovery is attributed to Robert Elderfield of Columbia University in the year 1946 and was part of a coordinated effort led by the OSRD (Office of Scientific Research and Development) to develop an anti-malarial drug for soldiers fighting in the Pacific Ocean Theater during World War II.
Primaquine is normally prescribed for regions where the principal malarial parasite is P. vivax (e.g. in parts of Asia and South America), although the medication also protects against P. falciparum, which is the more dominant strain in Africa.
The drug has the ability to kill the dormant stage of P.vivax that can live in the liver for months (or even years) and that often causes malaria relapse.
According to goodrx.com, the average retail price for a 1-month supply of thirty 26.3 mg adult tablets is $64.72, making it the third most inexpensive antimalarial drug on our list.
The recommended dosage for adults is 15 mg base (26.3 mg salt) taken daily and for children 0.5 mg base (0.8 mg salt) per kg taken daily.
This drug is a good choice for shorter trips because it only has to be taken for 7 days after the trip finishes. It’s also good for last-minute travel plans, as it only has to be taken 1-2 days before the trip commences.
There are some issues however with Primaquine.
Nausea, vomiting and stomach cramps are among the common side effects and the drug shouldn’t be taken by pregnant women or by those with G6PD (glucose-6-phosphatase-dehydrogenase) deficiency, nor by those who have not been tested for the condition.
G6PD deficiency is an inherited condition that mostly affects males, particularly those of African or Middle-Eastern descent.
The condition stems from an inadequate amount of the G6PD enzyme in the blood, which can result in red blood cells breaking down prematurely (hemolysis) when the body is exposed to various triggers including certain foods, drugs (e.g. Primaquine) and infections.
If the red blood cells are being destroyed faster than the body can replace them a condition called hemolytic anemia develops, which can be fatal if not properly treated.
Although there are costs and delays involved, it is advisable to get tested for G6PD deficiency before taking this drug. The good news is that the test only has to be performed once.
Another drawback with Primaquine is that it’s not safe for use with pregnant or breastfeeding women (unless the infant has been tested for G6PD deficiency).
Tafenoquine
Tafenoquine is a relatively new antimalarial drug related to Primaquine that in 2019 became the first drug in 18 years to be approved for malaria prevention by the FDA.
First discovered at the Walter Reed Army Institute of Research (WRAIR) back in 1978, the drug was further developed collaboratively by the British multinational pharmaceutical giant GlaxoSmithKline and Switzerland-based Medicines for Malaria Venture (MMV).
The latter is the leading product development partnership (PDP) in the field of antimalarial drug research and development.
Like Primaquine, Tafenoquine is prescribed for travellers visiting areas that are affected by P. vivax, as it has the ability to kill the parasite in its dormant liver stage and prevent malaria relapses. It also protects against P. falciparum.
The drug goes under the brand names Arakoda (60 degrees pharmaceuticals) and Krintafel (GlaxoSmithKline) and is technically classified as an 8-aminoquinoline.
The dosage for adults is 200 mg taken daily for 3 days before travel, taken weekly during travel and then taken just once after travel, making it a good choice for last-minute trips, short trips and longer trips.
The drug is not suitable for young children and should only be prescribed for persons aged 16 years or older.
Like Primaquine, Tafenoquine can cause hemolysis (premature red blood cell breakdown) in people with G6PD deficiency, so it shouldn’t be taken by those that have the condition or by those that haven’t been tested for it.
As with Primaquine, the drug is also unsafe for women that are pregnant or breastfeeding.
The drug may exacerbate or cause psychosis in some people, so those with psychiatric disorders should avoid it. Common side effects include diarrhea, nausea, vomiting, dizziness, back pain and also insomnia, nightmares, depression and anxiety.
Mosquitoes are a global nuisance and health risk that travellers are often tormented by.
Their high-pitched whine irritates, their bite causes itching and swelling and they often transmit potentially dangerous viruses and malaria parasites in their saliva.
As we’ve shown in this article however, there are a number of measures you can take to counter mosquitoes, thereby keeping them and the diseases they carry at bay.
Whether it’s chemoprophylaxis, mosquito bed nets or topical sprays, success in avoiding bites and minimizing the risk of falling ill largely depends on employing the appropriate measure for the situation, with a combination of methods often being the most effective.
Mosquitoes may be here to stay for good, so all we can do, at least for the time being, is learn how best to deal with them.
If you enjoyed this article or found it helpful, please share it with other travellers. How do you normally deal with those pesky mosquitoes when you're travelling? Please leave us a comment below and we'll get back to you as soon as we can!
You may also like:
JOIN OUR LIST
SUPPORT US
FOLLOW US
ABOUT US
Our names are Eoghan and Jili and we hail from Ireland and India respectively.
We are two ardent shoestring budget adventure travellers and have been travelling throughout Asia continuously for the past few years.
Having accrued such a wealth of stories and knowledge from our extraordinary and transformative journey, our mission is now to share everything we've experienced and all of the lessons we've learned with our readers.
Do make sure to subscribe above in order to receive our free e-mail updates and exclusive travel tips & hints. If you would like to learn more about our story, philosophy and mission, please visit our about page.
Never stop travelling!
FOLLOW US ON FACEBOOK
FOLLOW US ON PINTEREST
-lw-scaled.png.png)